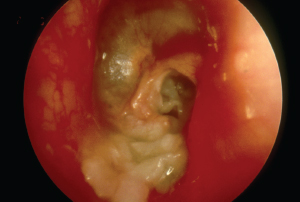
Otoscopic view of myringitis. Dr. Livingstone used a database of otoscopic images to train his algorithm to diagnose 14 otologic conditions.
© BSIP / Science Source
The program relies on artificial intelligence (AI) to optimally construct the neural network, he added. AI is rapidly expanding. Dr. Livingstone and his team built a hardware-agnostic algorithm using a database of 1,366 otoscopic images and trained it to diagnose 14 otologic conditions. The algorithm can also diagnose multiple conditions simultaneously (i.e., an extruded tympanostomy tube in a patient with a retraction and an effusion). The diagnostic threshold is set for each condition to optimize accuracy and patient safety. Using a test set of 89 algorithm-naïve images, the researchers obtained an average positive predictive value of 90.9% and a sensitivity of 86.1%.
Explore This Issue
July 2019In the study, 10 physicians (five junior otolaryngology residents, two general practitioners, one pediatric resident, one internal medicine resident, and one emergency medicine resident) were tested on the same 89 images. For nearly every diagnosis, the algorithm performed significantly better than the physicians, said Dr. Livingstone.
“This algorithm could be embedded into a digital otoscope platform to decrease healthcare costs and streamline the triage of consultations,” he added. “There is excellent potential for this algorithm in rural, remote, and low-resource health systems across the world.”
Departmental Education and Standardized Guidelines Decrease Number and Amount of Opioid Prescriptions
 To assess whether education and guidelines can reduce opioid prescribing, Katherine Lees, MD, chief resident at the Mayo Clinic in Rochester, Minn., undertook a project to address the prescribing practices of her department. “Recent evidence shows that 70% to 80% of the opioid pills we prescribe after surgery aren’t being used by patients,” she said. “When we examined the opioid prescribing practices of our department, we were fairly shocked by the amount and variability we found, likely due to the lack of clear evidence to guide our prescribing practices.”
To assess whether education and guidelines can reduce opioid prescribing, Katherine Lees, MD, chief resident at the Mayo Clinic in Rochester, Minn., undertook a project to address the prescribing practices of her department. “Recent evidence shows that 70% to 80% of the opioid pills we prescribe after surgery aren’t being used by patients,” she said. “When we examined the opioid prescribing practices of our department, we were fairly shocked by the amount and variability we found, likely due to the lack of clear evidence to guide our prescribing practices.”
She and her team developed standardized prescribing recommendations with the help of pharmacists, pain specialists, and similar initiatives from other surgical departments. They then provided formal opioid prescribing education at the department of otolaryngology grand rounds and introduced the guidelines.
The investigators compared the opioid prescription amounts and refill rates for a number of procedures before and after implementation of formal education and guidelines. Although there was no difference in the number of patients who received an opioid prescription, the team found that the amount of opioids prescribed decreased by about 50%—from 20 tabs of oxycodone to 10. There was also a decrease in variability of these prescriptions among providers. Importantly, she added, there was no change in the refill rates, suggesting that, even though practitioners are prescribing less, patients still experienced adequate pain management.
“We’ve expanded our guidelines to the otolaryngology departments at Mayo in Florida and Arizona, and will continue to make adjustments to the guidelines based on patient and provider feedback,” she said. “This has just been the first step in changing how we manage patients’ pain after surgery, but so far it has been very well received by our practitioners and patients alike.”