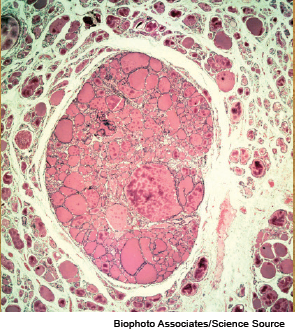
Light micrograph of a section through a thyroid gland with a colloid adenoma.
ORLANDO—Thyroid nodules that are not clearly benign or malignant make for a thorny issue for head and neck surgeons. When diagnostic surgery is performed, the nodules often turn out to be benign.
An expert panel at the AAO-HNS Annual Meeting discussed new approaches that are being developed and gradually making their way into wider use to help to better assess these nodules and tailor care to the individual.
Robert Ferris, MD, PhD, chief of head and neck surgery at the University of Pittsburgh Cancer Institute, said molecular testing of thyroid nodules is becoming an increasingly useful tool in helping head and neck surgeons make surgery decisions in a personalized way when cytology yields unclear results. The approach, currently being fine-tuned by Yuri Nikiforov, MD, PhD, in the division of molecular anatomic pathology at the University of Pittsburgh School of Medicine, involves testing for mutations in a panel of genes. At Pittsburgh, this testing has been used since 2007.
Gradually, the test has been strengthened to yield more useful results. Using a seven-gene panel, the positive predictive value for follicular lesions of undetermined significance (FLUS) was an acceptable 88%, and the negative predictive value was 94%, leaving otolaryngologists comfortable observing nodules in the remaining 6% rather than jumping to diagnostic surgery.
But the negative predictive values for other indeterminate nodules—follicular neoplasms (FN) and those deemed suspicious for malignant cells (SMC)—were less desirable, at 86% and 72%. That’s too high to simply observe those patients, Dr. Ferris said, noting that by adding genes to the test and using a 12-panel assessment, the negative predictive values—for follicular neoplasms and SMC nodules taken together—have increased to 96%, with the positive predictive value remaining high at 83%.
Dr. Ferris said he thinks they’ve reached the point at which the negative predictive values allow observation rather than surgery in those with negative results. He stressed, however, that the positive and negative predictive values fluctuate depending on the prevalence of malignancy at a given institution, so it is crucial to know that number. “You should not use a molecular test unless you know in your own institution the rate and prevalence of malignancy in that category,” he said.
Rule-Out Test
Robert Witt, MD, professor of otolaryngology-head and neck surgery at Thomas Jefferson University in Philadelphia, said that another new approach—the Afirma Gene Expression Classifier (GEC)—is strong in its negative predictive value and is powerful as a “rule out” test. The test measures the expression of 142 genes from a fine needle aspiration sample to determine whether a nodule originally deemed indeterminate on cytopathology is benign or suspicious.
The test holds great potential to reduce the number of unnecessary diagnostic surgeries, Dr. Witt said. Traditionally, 15% to 25% of nodules are classified as indeterminate, and subsequently, approximately 80% of those are found to be benign.
Diagnostic thyroid surgeries come with drawbacks: They cost $6,000 to $10,000, involve the possibility of complications, often mean lost time from work and difficulty meeting daily responsibilities, and cause anxiety and possible iatrogenic hypothyroidism and lifelong medications, he said. “One could say in retrospect that most of these patients underwent unnecessary surgery,” he said. “We do have a better test, and we have it now.”
Across many studies, the negative predictive value of the Afirma test has been approximately 95% for FLUS and 94% for FN.
Context is Everything
Greg Randolph MD, associate professor of otology and laryngology at Harvard Medical School in Boston, underscored the importance of using genetic tests in the right context. The Afirma GEC works best in categories with a low prevalence of malignancy, for example, and the Asuragen oncogene panel works best when prevalence is higher.
He also emphasized, along with the others, that there is “tremendous, tremendous divergence” in the prevalence of malignancy from center to center—25% prevalence in one center for one type of nodule might be almost 50% in another. The correct use of the testing depends on those numbers.
Generally, nodules that are in the Bethesda categories of atypia of undetermined significance (AUS), FLUS, and FN would be more likely to undergo GEC testing. And those in the SMC category would be better suited for the oncogene panel. “[That] is how these tests are typically applied,” Dr. Randolph said. “Most would agree. There’s some debate, but most would agree.”
These tests are not the only factor to consider, though. In cases involving a well-informed patient who wants surgery and has a higher chance of malignancy due to vocal fold paralysis, a suspicious ultrasound finding, or other factors, surgery might be warranted with no need for testing.
He also stressed the importance of patient consultation in cases of thyroid surgery. “I think it’s important to take time with these patients,” he said. “Every patient that I see who I know will need surgery, I force them to see me twice. This is not the most convenient or time-efficient way to run a practice, but it allows you to see the patient initially and see the patient a second time for a pre-operative visit, and it allows an agenda matching. With that amount of time, you never get a patient saying, ‘You told me I had a tumor. I thought it was a cancer.’”
Ready for Mainstream?
Edmund Pribitkin, MD, vice chair of otolaryngology-head and neck surgery at Jefferson Thyroid and Parathyroid Center in Philadelphia, said that while the rate of thyroid cancer diagnoses has been increasing, the mortality rate has been level. “People aren’t dying, necessarily, of the disease, even though it’s being discovered more often in folks,” he said.
—Edmund Pribitkin, MD
So when otolaryngologists are considering expensive genetic testing, they need to make sure it’s worth it. “If we’re going to do this testing, we need to make sure that it affects our decision making in terms of caring for folks,” he said. “Identification of risk does not really guarantee a benefit of treatment.”
Dr. Witt said that it’s an exciting time in thyroid surgery. “Few fields in medicine rival the dynamism of modern thyroid diagnosis, management, and prognostication,” he said. “Molecular alteration testing, next generation sequencing, and gene expression classifier testing are the most important advances in the diagnosis and management of cancer since the introduction of fine needle aspiration cytology a half-century ago.”
Keith Forwith, MD, PhD, an otolaryngologist at Advanced ENT and Allergy in Louisville, Ky., who sat in on the session, said some of the tests “aren’t ready for mainstream private practice outside of an academic setting, but they’re getting closer.” Afirma is now widely available, and he’s used it some, but he added, “Some of the patients that I’ve done it on have been hit with a $1,400 bill, so you have to be careful about whether that’s covered or not covered.” Also, whether to use such testing has to depend in part on the sophistication of the patient, he said. “This is not for an uneducated patient who has difficulty sorting through the science of it.”