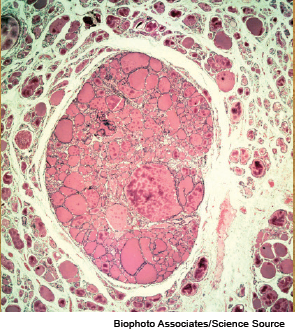
Light micrograph of a section through a thyroid gland with a colloid adenoma.
ORLANDO—Thyroid nodules that are not clearly benign or malignant make for a thorny issue for head and neck surgeons. When diagnostic surgery is performed, the nodules often turn out to be benign.
Explore This Issue
November 2014An expert panel at the AAO-HNS Annual Meeting discussed new approaches that are being developed and gradually making their way into wider use to help to better assess these nodules and tailor care to the individual.
Robert Ferris, MD, PhD, chief of head and neck surgery at the University of Pittsburgh Cancer Institute, said molecular testing of thyroid nodules is becoming an increasingly useful tool in helping head and neck surgeons make surgery decisions in a personalized way when cytology yields unclear results. The approach, currently being fine-tuned by Yuri Nikiforov, MD, PhD, in the division of molecular anatomic pathology at the University of Pittsburgh School of Medicine, involves testing for mutations in a panel of genes. At Pittsburgh, this testing has been used since 2007.
Gradually, the test has been strengthened to yield more useful results. Using a seven-gene panel, the positive predictive value for follicular lesions of undetermined significance (FLUS) was an acceptable 88%, and the negative predictive value was 94%, leaving otolaryngologists comfortable observing nodules in the remaining 6% rather than jumping to diagnostic surgery.
But the negative predictive values for other indeterminate nodules—follicular neoplasms (FN) and those deemed suspicious for malignant cells (SMC)—were less desirable, at 86% and 72%. That’s too high to simply observe those patients, Dr. Ferris said, noting that by adding genes to the test and using a 12-panel assessment, the negative predictive values—for follicular neoplasms and SMC nodules taken together—have increased to 96%, with the positive predictive value remaining high at 83%.
Dr. Ferris said he thinks they’ve reached the point at which the negative predictive values allow observation rather than surgery in those with negative results. He stressed, however, that the positive and negative predictive values fluctuate depending on the prevalence of malignancy at a given institution, so it is crucial to know that number. “You should not use a molecular test unless you know in your own institution the rate and prevalence of malignancy in that category,” he said.
Rule-Out Test
Robert Witt, MD, professor of otolaryngology-head and neck surgery at Thomas Jefferson University in Philadelphia, said that another new approach—the Afirma Gene Expression Classifier (GEC)—is strong in its negative predictive value and is powerful as a “rule out” test. The test measures the expression of 142 genes from a fine needle aspiration sample to determine whether a nodule originally deemed indeterminate on cytopathology is benign or suspicious.