What complex interdisciplinary decision making and modern endovascular techniques go into the management of patients with carotid blowout syndrome (CBS)?
Bottom line
Modern endovascular approaches for acute CBS management yield optimal results and should be used in a coordinated manner by the head and neck surgeon and the neurointerventionalist using a stepwise approach.
Explore This Issue
February 2017Background: CBS, a complication of head and neck cancer and treatment, encompasses three distinct clinical entities: threatened, impending, and acute carotid blowout. Current CBS management strategies involve endovascular approaches. Nationwide trends of these strategies show proportionally higher use of endovascular sacrifice (88.6%) compared with covered stenting (11.4%) in acute CBS management, while overall mortality rates and acute ischemic stroke rates are reported as similar for both.
Study design: Retrospective chart review of 33 patients who had 38 hemorrhagic events related to head and neck cancer that were managed with endovascular means between 2004 and 2014.
Setting: University Hospitals Case Medical Center, Cleveland, Ohio.
Synopsis: In all patients, the lingual branch of the external carotid artery (ECA) was most commonly involved (47.8% of ECA branch cases); multiple branches were involved in 30.4% of cases and included complex blood supply from the lingual-facial trunk and branches originating from the superior thyroid and inferior thyroid arteries. In all such cases, embolization (coil embolization and/or PVA particles) was used successfully with resultant complete control of hemorrhage. Fifteen procedures were related to great vessel hemorrhage; of these events, five were localized to the ECA trunk, and in all cases successful control was achieved using embolization.
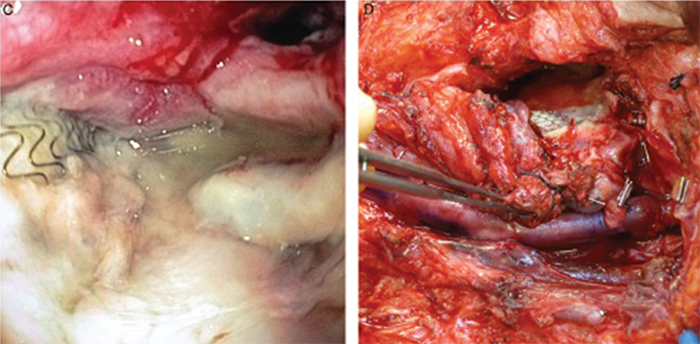
Figure 1. (C) Direct pharyngoscopy showing exposed covered stent in the pharynx. (D) Definitive vascular reconstruction of the left carotid artery with superficial femoral vein graft.
Credit: Copyright 2016 The American Laryngological, Rhinological and Otological Society, Inc.
Three cases were presented in depth:
Case 1 involved a 66-year-old male with prior left oropharyngeal squamous cell cancer presenting with a left neck abscess involving the carotid space. Endovascular management resulted in a complete and rapid hemorrhage resolution with no neurological deficits.
Case 2 involved a 52-year-old male with recurrent supraglottic squamous cell cancer presenting with a large right pharyngocutaneous fistula with exposed carotid artery one month after salvage laryngectomy and reconstruction. He had no recurrence or rebleed 18 months following endovascular sacrifice of CCA and embolization.
Case 3 involved a 63-year-old female with prior history of multiple laryngeal primary cancers who underwent salvage laryngectomy. After 19 years disease free, she presented with an episode of sentinel bleed. Following multiple diagnoses and procedures, she was 16 months post-acute CBS status without neurological deficit or recurrent disease.
Citation: Manzoor NF, Rezaee RP, Ray A. Contemporary management of carotid blowout syndrome utilizing endovascular techniques. Laryngoscope. 2017;127:383-390.