According to the authors, “the ability to return to the same location and limiting the scope of the mission to ear disease gave the unique opportunity to collect data, evaluate results, and quantify patient benefits.”
Explore This Issue
December 2010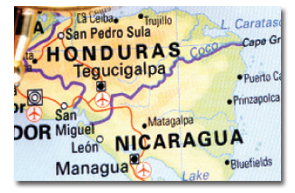
Follow-up and Training
While programs are beginning to quantify their missions abroad using data analysis, some missions continue to measure their successes through individual patient follow-up and local doctor training.
“Many of us have long-standing relationships with providers in local countries, and so we get feedback on our patients there as well as here. It’s not a whole lot different than how we measure outcomes here at home, which is to say we don’t,” said Dr. Saunders, whose Mayflower Medical Outreach program runs trips to Nicaragua about twice a year.
Dr. Saunders said the rate of success is much higher abroad when the procedure has been proven successful in the U.S. “The greatest need and the thing we’re focused on is ear surgery,” he said. “Ear disease is the most rampant untreated part of otolaryngology in that part of the world, and also pretty much true around the world. It’s fortunate for me because that’s where my expertise is. What they needed is what I had to offer.”

Procedures like cochlear implants, according to Dr. Saunders, are more difficult to do on missions, although the need is there. “Those are highly technical procedures with the need for a tremendous amount of peripheral support, and clearly that’s a place where you have to have that kind of long-term relationship and really have some good outcome measures,” he said.
Dr. Horlbeck said volunteers should avoid procedures that require ICU stays.
And, according to a recent editorial in the World Journal of Surgery about the “sins” of humanitarian work, “One good rule is to offer the types of procedures that are minimally invasive, to relieve immediate discomfort, and that require little follow-up care, especially for missions that are short-term” (World J Surg. 2010 34(3):466-470).
For Dr. Woodson, training local physicians is the “major outcome variable” of her missions abroad. Twice a year, Dr. Woodson travels to Kilimanjaro Christian Medical Centre in Moshi, Tanzania, where she and other otolaryngologists and audiologists treat a variety of problems, including meningocele, laryngeal cancer, papilloma, parotid tumors, tracheal and glottic stenosis and laryngeal paralysis. “When we went to Tanzania, people were dying from laryngeal cancer, who could have been cured by laryngectomy. We resolved to teach the local doctors how to take care of these people,” she said.
Leave a Reply