What happened on Thursday, April 16, was nearly two decades in the making. After 18 years and 17 short-term patches, President Obama signed a $214 billion Medicare reform package (HR 2) that addresses issues that have long plagued physicians and their patients. Dubbed the “doc fix,” the Medicare Access and CHIP Reauthorization Act (MACRA) permanently ends yearly threats to cut Medicare payments to physicians, a practice that stems back to a 1997 law.
Explore This Issue
June 2015“We are very excited about it,” said James C. Denneny III, MD, executive vice president and CEO of the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS), who has been lobbying, along with other members of the organization, to get the bill passed for 14 years. “It is very gratifying to have it finally come to fruition,” he added.
But Dr. Denneny was quick to note another aspect of the victory—its strong bipartisan support. The U.S. Senate passed the bill by a vote of 92-8, and the House approved it by a 392-37 vote. “The scope of this bill underscores what can be accomplished when lawmakers work in a bipartisan manner,” Dr. Denneny said. “To see the system work was very important to me.”
Jeffrey Kahn, MD, an otolaryngologist at the Texas-based Austin Ear Nose and Throat Clinic who serves on the Texas Medical Association’s Council on Health Care Quality, acknowledged the amount of effort that went into the bill’s passage. “It’s great that it passed, but it seems a bit like a hollow victory because so much work and resources went into fixing something that should have been fixed long ago and that clearly had broad bipartisan support.”
The Nuts and Bolts
The Medicare physician payment provisions are expected to help build a more sustainable, fair, and efficient Medicare physician payment system that results in high quality, affordable healthcare. The bill, negotiated by House Speaker John Boehner and House Democratic Leader Nancy Pelosi, calls for spending $214 billion over 10 years, with $73 billion offset by spending cuts or new revenue.
The new law includes provisions that address several legislative priorities set forth by the AAO-HNS. Among these are the permanent repeal of the flawed sustainable growth rate (SGR) formula used to determine payments to physicians under the Medicare program. “This represents a great improvement in Medicare payment for patients and physicians,” said Gregory W. Randolph, MD, director of the general otolaryngology and thyroid surgical divisions at Massachusetts Eye and Ear Infirmary and Harvard Medical School, Boston. “As a result of this, a 21.2% physician pay cut was avoided.”
 We’d better get the value-based issue right; if we don’t, it could adversely change the whole landscape of medicine and our relationship with our patients.
We’d better get the value-based issue right; if we don’t, it could adversely change the whole landscape of medicine and our relationship with our patients.—Jeffrey Kahn, MD
The flawed payment formula has caused ongoing uncertainty with regard to whether or not physicians could profitably take on Medicare patients. “Several colleagues were concerned that their salary may be cut when it seemed like the cuts would actually go through,” Dr. Randolph said. “For private practitioners, it must have been even more stressful, as it would directly and immediately cut their take-home pay and affect their practice’s cash flow.”
Dr. Denneny said that while the patches were aimed at preventing marked decreases in physician payments, the new legislation now allows for stability in Medicare payments. “Knowing that they won’t face huge cuts will allow practitioners to expand their practices by buying new technology or equipment or offering new services that will improve patient care,” he says.

The new legislation is expected to help build a more efficient, sustainable, and fair Medicare physician payment system.
The legislation also repeals the recent Centers for Medicare and Medicaid Services policy to transition all 10- and 90-day global payment codes to zero-day codes by 2018. “Within the bill, MACRA mandates that CMS produce data in 2017 before proceeding with this,” Dr. Denneny said. “This particular mandate by CMS last year was potentially devastating if the same process was also implemented in the private payer market. Patients could be faced with multiple copays for hospital visits and post-operative visits—which some people couldn’t afford. As a specialty, we felt that this would decrease the quality of care and didn’t fit in with the direction of healthcare reform.”
Quality Reporting Overhaul
The new legislation also consolidates three existing performance-based programs (the EHR meaningful use incentive program, the Physician Quality Reporting System, and the value-based payment modifier established under the Affordable Care Act) into a unified Merit-based Incentive Payment System (MIPS). “Physician payment will no longer be based solely on the volume of services, but also on the quality and value of physician’s care,” said Dr. Randolph.
Dr. Denneny believes that MACRA-mandated consolidation of the existing performance-based programs in Medicare will simplify the quality reporting process. MIPS will evaluate performance of physicians in four categories: quality of care, resource use, meaningful use, and clinical practice improvements (see “MIPS Performance Category Weights,”).
The legislation also allows providers who participate in alternative payment models to opt out of MIPS.
AAO-HNS has guidelines that outline standards of care for otolaryngology-specific disease processes and is creating metrics that can be used to define, measure, and report otolaryngologic quality. “This work is epitomized by the academy’s new initiative to form an otolaryngology registry to provide quality metrics,” Dr. Randolph said. “It is essential for otolaryngologists to participate in this process in order to define quality in a way that truly makes sense within our field.”
MACRA allows Qualified Clinical Data Registries (QCDR) to be used to report quality measures under the new MIPS program, Dr. Denneny said. “MACRA codifies the fact that we will be able to use QCDRs for quality reporting. This is extremely important, given the fact that we are proceeding with the formation of our own QCDR,” he added.
Dr. Denneny also said that organization members will be able to report quality through one consolidated reporting system, which will minimize the effort to participate. “This will make it less likely for providers to be faced with penalties, which could increase by almost 10% over the next few years.”
He highlighted the fact that MACRA instructs the U.S. Secretary of Health and Human Services to provide $15 million a year to produce new quality measures. “For smaller specialties, this is quite a burden,” he said. “So we hope to apply for some of that money.”
Finally, in January 2015, CMS stated that 50% of providers will have to participate in alternate payment mechanisms by 2016 and 80% by 2018. “The law will allow for increased payments for these providers,” Dr. Denneny said. Physicians will earn a 5% bonus if they participate in new payment models that seek to improve care coordination from 2019 to 2024. Accountable care organizations (ACOs) will be incentivized to receive a set fee to take care of patients while meeting certain quality standards. The U.S. Department of Health and Human Services will ultimately determine these medical standards.
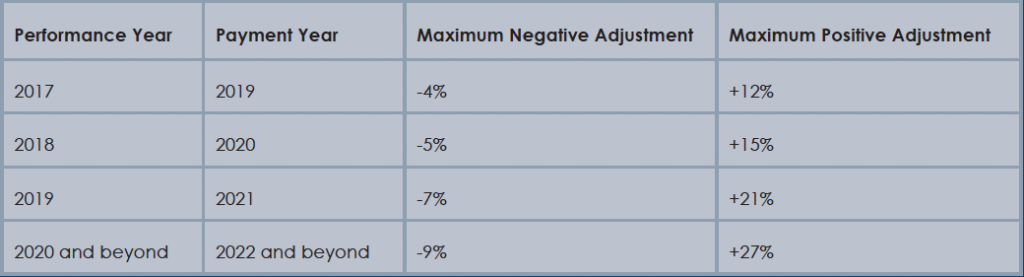
Physician payment adjustments under MACRA.
(Click for larger image) Physician payment adjustments under MACRA.
Source: Healthcare Information and Management Systems Society
What’s Next
As the new program gets underway, Dr. Denneny foresees a lot of opportunities, but much work still has to be done, and questions remain.
As the field of medicine moves toward a value-based payment system, Dr. Kahn said it is critically important that we figure out how to structure it. Quality and value are very important goals to work toward. “However, considering it took 17 years to fix the flawed Medicare formula, we’d better get the value-based issue right. If we don’t, it could adversely change the whole landscape of medicine and our relationship with our patients,” he said. “The big question will be how to define quality. It’s important that we don’t just create a definition simply to have any definition that will meet the deadlines set by the recent legislation.”
Dr. Randolph said that questions also remain regarding physicians who see lower patient volume and who may find it more difficult to provide quality data. In addition, there are questions concerning how scores of quality can be adjusted when patients who have more significant comorbidities receive care.
On another note, Dr. Kahn points out that third-party payers, such as Aetna, Blue Cross, and United Healthcare, tend to have a history of following the rules that Medicare sets. “So the law could have a broader effect if other payers begin to adopt what Medicare does with value-based payments,” he said.
A stressful annual ritual of physician payment cuts has finally come to an end. “It is gratifying to see the persistency of the message, the accuracy of the message, and the patience of so many to press onward to benefit the Medicare population,” Dr. Denneny said. “Now we can concentrate on other issues for patient care, instead of worrying about the funding.”
Karen Appold is a freelance medical writer based in Pennsylvania.