Dr. Denneny also said that organization members will be able to report quality through one consolidated reporting system, which will minimize the effort to participate. “This will make it less likely for providers to be faced with penalties, which could increase by almost 10% over the next few years.”
Explore This Issue
June 2015He highlighted the fact that MACRA instructs the U.S. Secretary of Health and Human Services to provide $15 million a year to produce new quality measures. “For smaller specialties, this is quite a burden,” he said. “So we hope to apply for some of that money.”
Finally, in January 2015, CMS stated that 50% of providers will have to participate in alternate payment mechanisms by 2016 and 80% by 2018. “The law will allow for increased payments for these providers,” Dr. Denneny said. Physicians will earn a 5% bonus if they participate in new payment models that seek to improve care coordination from 2019 to 2024. Accountable care organizations (ACOs) will be incentivized to receive a set fee to take care of patients while meeting certain quality standards. The U.S. Department of Health and Human Services will ultimately determine these medical standards.
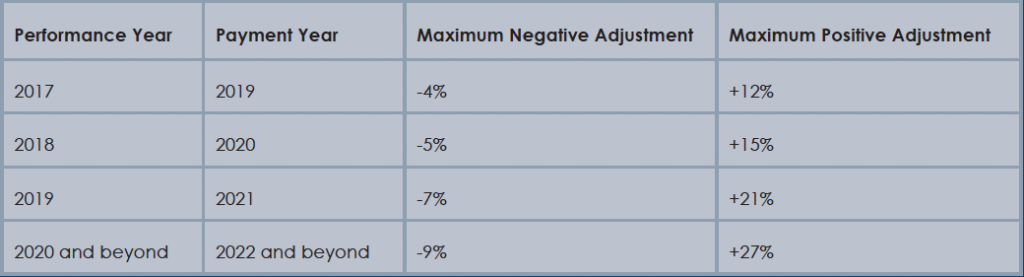
Physician payment adjustments under MACRA.
(Click for larger image) Physician payment adjustments under MACRA.
Source: Healthcare Information and Management Systems Society
What’s Next
As the new program gets underway, Dr. Denneny foresees a lot of opportunities, but much work still has to be done, and questions remain.
As the field of medicine moves toward a value-based payment system, Dr. Kahn said it is critically important that we figure out how to structure it. Quality and value are very important goals to work toward. “However, considering it took 17 years to fix the flawed Medicare formula, we’d better get the value-based issue right. If we don’t, it could adversely change the whole landscape of medicine and our relationship with our patients,” he said. “The big question will be how to define quality. It’s important that we don’t just create a definition simply to have any definition that will meet the deadlines set by the recent legislation.”
Dr. Randolph said that questions also remain regarding physicians who see lower patient volume and who may find it more difficult to provide quality data. In addition, there are questions concerning how scores of quality can be adjusted when patients who have more significant comorbidities receive care.
On another note, Dr. Kahn points out that third-party payers, such as Aetna, Blue Cross, and United Healthcare, tend to have a history of following the rules that Medicare sets. “So the law could have a broader effect if other payers begin to adopt what Medicare does with value-based payments,” he said.