Medical groups now are focused on a stand-alone Medicare physician payment reform bill sponsored by Rep. John D. Dingell, D-Mich. The measure is supported by the AMA, the American Academy of Otolaryngology—Head and Neck Surgery (AAO-HNS), and more than 100 other physician organizations. It would make the 2010 physician payment update equal to the increase in the Medicare Economic Index, a measure of inflation. That would translate into a 1.2 percent increase.
Explore This Issue
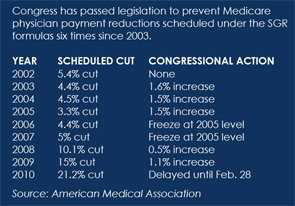
January 2010The bill, H.R. 3961, also would change the baseline on which the payment formula is computed. This would create a clean slate for future payment update calculations, thus wiping away the “debt” caused by the current formula.
The legislation would create two new spending targets, one for evaluation and management and preventive services and the other for all remaining services. The target growth rate for evaluation and management (E&M) and preventive services would be the gross domestic product plus 2 percent, while the target for other services would be GDP plus 1 percent. The change would reduce the likelihood of future physician payment cuts because the target growth rates would be more generous, according to the House Energy and Commerce Committee.
Senate Effort Fails
On the Senate side, a stand-alone Medicare physician payment bill in October failed on a procedural vote. That measure would have repealed the SGR formula and set future Medicare physician payment updates at zero. The legislation, sponsored by Sen. Debbie Stabenow, D-Mich., would have laid “the foundation for establishing a new Medicare physician payment update system through health system reform or other legislation,” according to the AMA.
At press time, Senate Majority Leader Harry Reid, D-Nev., was still working on merging health system reform bills passed earlier this year by the Senate Finance Committee and the Health, Education, Labor and Pensions Committee. The Finance Committee bill contains several Medicare payment provisions that trouble physician organizations. Its 0.5 percent Medicare physician payment increase in 2010 falls short of permanent repeal of the flawed formula.
Another temporary increase would amount to lawmakers kicking the problem down the road again, Dr. Kuppersmith said. A 0.5 percent increase, like the past temporary payment fixes, would not keep up with costs, he said. “It’s still a pay cut because my utility bill goes up. I have to give employees cost of living increases. None of my costs are coming down, and they’re all going up more than 0.5 percent,” said Dr. Kuppersmith, who is president of the AAO-HNS Board of Directors.
Leave a Reply