“What are the periop and postop risks?” I asked.
Explore This Issue
June 2022“Death, stroke, paralysis, but all are extremely rare. Also there’s a 1% to 2% chance you’ll have permanent hoarseness if the recurrent laryngeal nerve is impacted, but I think ENTs can do something about that. You’ll have severe throat pain like a tonsillectomy for up to two weeks, sometimes longer. After maybe four weeks, it should get better. You may have the sensation that something is stuck in the throat, called globus, for a while, but it goes away.”
“What about range of motion?” I persisted.
“Oh, yes; you’ll lose about 15 degrees, so you won’t be able to touch your chin to your shoulder on either side.”
“I’m not sure I want to take these risks now, not yet,” I said softly. “
You’re okay. You can live with this. Let’s try one more cervical epidural injection, and if you get worse, call me and we can set up surgery.”
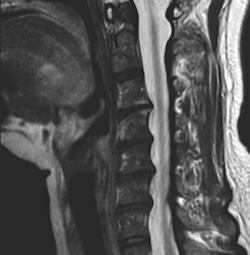
The next day, my orthopedic surgeon was quite concerned. “I looked at your MRI myself, and it’s pretty bad,” he said. “Here’s where it’s severely stenotic and why you developed radiculopathy.”
I shared the recommendation from the neurosurgeon, and the orthopedic surgeon said quickly, “Oh, don’t have that surgery. My father did, and he couldn’t swallow for six months; he aspirated everything and needed a feeding tube. It was awful. They ended up taking the plate out, and he was able to swallow again.”
He injected my shoulder with Kenalog and Marcaine again to try and improve the adhesive capsulitis and range of motion. Leaving his busy office, with countless people in his waiting room, I held back the tears. If I had started, I might not have been able to stop.
Going on Leave
The six weeks leading up to my leave were a blur. I had tried to make up my scheduled calls to minimize the impact to my partners, despite their willingness to do more. My entire team and clinical staff were beyond supportive while I agonized over the guilt, shame, and uncertainty for my life and surgical career, and wondered if I could avoid surgery. Once on leave, I had two episodes of neurogenic vasoconstriction, with my right hand turning blue and ashen gray (like a corpse) for five to 10 minutes, on and off. All I could do was breathe and stay calm until it went away.