With the availability of noninvasive procedures that use injectable fillers to do the work surgery once monopolized, more people than ever before are seeking the elixir of youth that comes now at the end of a needle rather than a knife.
For the physicians who wield this needle, communicating the risks of injectable fillers is critical, both to inform the patient of any potential negative outcomes and to modulate the patient’s expectation of what fillers can and cannot do about what nature has either eroded or neglected to give.
Along with educating patients about the number of products available and safely administering the product, Jonathan Sykes, MD, professor and director of facial plastic and reconstructive surgery at the University of California (UC) Davis Medical Center in Sacramento, Calif., and president-elect of the American Academy of Facial Plastic and Reconstructive Surgery, emphasized that his job also involves talking about limitations. “There are some patients who want something that won’t work, or it may take more than one injection” he said. “My job is to provide two-way communication to find out what the patient wants.”
What the Patient Wants
Finding out what the patient wants is the first step in discussing the potential risks of fillers, because not fulfilling patient expectations is one of the risks.
“The first thing I try to do with patients is to get a concept of what they want to accomplish and what timeline they want to accomplish that in,” Dr. Sykes said.
Knowing the overall goals of each patient provides the foundation on which to discuss which fillers may or may not be appropriate and the potential risks of various fillers based on the agent used as well as their longevity (See “Complications of Injectble Fillers,” page 21).
“I listen to what concerns the patient, and if a filler is appropriate, I explain both the risks and the benefits,” said Hayes Gladstone, MD, associate professor and director of dermatologic surgery at the Stanford University School of Medicine in Stanford, Calif. For example, he said, if the patient wants lip augmentation, filler with hyluronic acid or collagen may be appropriate, while calcium hydroxylapatite could lead to lumpiness.
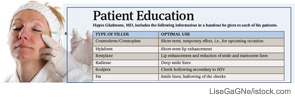
After selecting the appropriate filler and procedure, Dr. Gladstone then discusses with the patient the risks and benefits and provides a handout detailing these as well as the procedure itself. Included in the handout is a description of the most common fillers used and what they are best used for (see “Patient Education,” p. 21). When the patient comes in for the procedure, Dr. Gladstone again discusses the risks and benefits.
For Dr. Gladstone, ensuring clear communication with the patient goes beyond simply describing the fillers and their use. Fundamentally, it includes an overall philosophy of facial rejuvenation. Recounting an experience with a patient who was focused only on correcting her smile lines, despite his suggestion that she could benefit from a more global volumization of her face, he said he reluctantly followed her lead and only used a filler to correct her smile lines. “She was disappointed because her overall appearance, in terms of rejuvenation, was very small, and yet she had spent several hundred dollars,” he said. “That taught me to really communicate to the patient that it is not just about filling lines, as well as the need to make sure all questions are answered.”
Personalized Fillers
Along with identifying which particular filler is appropriate for each patient’s need, Dr. Gladstone also stressed the importance of making sure that the patient is appropriate for the filler. Because these are elective procedures, he is cautious about performing them on patients with serious acute illnesses or infections but makes this decision on a case-by-case basis.
“Obviously, we use fillers for HIV associated with lipoatrophy, and the patients are fine,” he said; however, he cautioned that patients who are immunocompromised are at a higher risk of infection. In addition, Dr. Gladstone does not perform cosmetic procedures on pregnant women. “Although the risks to the fetus are probably low,” he said, “I don’t know for sure, and therefore I take a conservative approach.”
Certain patients also need to be aware of their increased risk. Lisa Danielle Grunebaum, MD, assistant professor of otolaryngology/facial plastic and reconstructive surgery and co-director of the University of Miami Miller School of Medicine’s Cosmetic Medicine Group in Miami, Fla., said these patients include those with severe or complicated medical problems, including autoimmune and rheumatologic disorders, elderly patients, those on blood thinners and possibly those who have undergone previous facial surgery.
This last group, she said, may be at increased risk of more serious complications. “I believe that patients who have undergone previous facial surgery, such as rhinoplasty, may be at greater risk for necrosis due to possible interruption of collateral blood supply,” she added.
Other serious risks, however rare, include delayed complications such as granulomas and infection. Recent reports suggest that the development of biofilms may be an underlying cause of these rare complications (Plast Reconstr Surg. 2010;125(4):1250-1256). Although associated more with long-term fillers, biofilms can be seen with almost any filler, according to Rod J. Rohrich, MD, professor and chairman of plastic surgery at the University of Texas Southwestern Medical Center in Dallas. Dr. Rohrich stressed the importance of informing patients that, if they occur, it takes anywhere from weeks to months for biofilms to resolve completely.
Discussing Cost
Because cosmetic procedures are elective, the role of cost in a patient’s decision of which inflatable filler to use may be an important factor in discussing the overall cost-benefit ratio of each filler.
“Price can certainly play a role in the decision-making process,” said Sukhjit Johl, MD, senior physician of oculoplastic surgery at The Permanente Medical Group, Inc., in Sacramento, Calif. “But I would not agree to do something if I felt it was harmful or unlikely to accomplish what the patient expects.”
To ensure patients’ understanding of the risks and benefits, Dr. Johl has a thorough discussion with each patient prior to any procedure to make sure the patient has a realistic idea of how much filler volume will be required to achieve the desired result. He uses standardized pictures provided by the manufacturers that show the effects of different volumes of filler for a given patient. For example, manufacturers of Restylane provide pictures showing a patient before and after injection of 1 ml and 2 ml of Restylane in the nasolabial folds, he said.
When two fillers are thought to have a similar benefit, Dr. Gladstone gives the patient the choice. “Usually the filler that doesn’t last as long will cost less,” he said, adding that he encourages the shorter-acting and less expensive filler for patients trying a filler for the first time.
Long-Lasting Results vs. Permanent Problems
It is particularly important to make sure that patients who want longer-lasting fillers, such as polymethyl methacrylate and silicone (permanent fillers) and poly-L-lactic acid (Sculptra), are aware of the potential risk for complications, which include granulomas and infection.
Wendy W. Lee, MD, assistant professor of clinical ophthalmology at the University of Miami’s Miller School of Medicine, emphasized the need to let patients know that complications from these fillers may require surgical excision.
“If overinjected, permanent fillers will be more apparent and not go away completely without surgical excision,” she said. “As well, if a patient has a hypersensitivity reaction or other complication, surgical excision of the permanent filler may need to be performed.”
Dr. Lee also cautioned that one of the difficulties with long-term or permanent fillers is that as the face continues to age, previously injected permanent fillers may become apparent in unwanted ways.
Because of the risk of permanent problems, Dr. Sykes doesn’t use permanent fillers. “There are a lot of people who use them and are successful with them, but I realize that any negativity that you get by overinjecting an area or nodule with a long-term filler is a permanent result, and that is a problem,” he said.
Dr. Sykes prefers to use poly-L-lactic acid, which he calls an intermediate filler; unlike permanent fillers, it won’t introduce the potential for a permanent unwanted result. “I love it,” he said. “I think it is a safe product, and it has nice long-term results with global volumization.”
He does caution patients, however, that there is a greater propensity for papule and nodule formation with this type of filler if it is injected too superficially. But this can be avoided if it is mixed correctly and injected more deeply than shorter-term fillers, he said.
Dr. Grunebaum also avoids permanent fillers; instead, she uses calcium hydroxylapatite (Radiesse) for facial remodeling. “In the right patient, I feel that it has the best consistency for lasting and reliable mid-face augmentation,” she said.
Overall, Dr. Gladstone emphasized that “the philosophy is to volumize the face, [which means] looking at the aging face as a whole rather than just filling specific lines.” He said short- or medium-term acting fillers may be better than long-term fillers to manage the face changes that occur because of aging.
Despite the low incidence of risk, however, all agree that it is critical to talk frankly to each patient about potential risks, including the risk of not meeting patient expectations.
“A patient’s happiness after a procedure is equal to the outcome minus their expectations,” said Dr. Johl, who recommends taking pictures prior to the procedure so that patients can compare these to the outcomes.
Leave a Reply