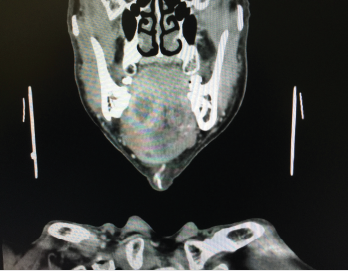
This CT scan shows a large abscess inside the tongue tissue.
©Karan Bunjean / shutterstock.com
It’s been nearly four years since the American Joint Committee on Cancer (AJCC) updated the staging system for oral cavity squamous cell carcinoma (OCSCC). Key revisions include factoring in depth of invasion (DOI) and extranodal extension (ENE) of the primary tumor (AJCC Cancer Staging Manual. 8th ed. Springer International Publishing: American Joint Commission on Cancer; 2017).
Explore This Issue
October 2021Although more work needs to be done to incorporate the AJCC8 staging system into clinical practice, it has already had an impact on more accurate staging of primary tumors, thus opening the door for better risk stratification and treatment, according to several head and neck cancer specialists.
The stakes for accurately staging OCSCC are high, given its high incidence and poor prognosis. The condition remains one of the most common cancers in the United States, affecting approximately 34,000 people each year. Five-year survival for patients with localized disease is approximately 75%; however, when the cancer has spread to the lymph nodes, survival rates drop to about 50%.
“We’ve all recognized for a while that the DOI of an oral cavity cancer is a very significant prognostic indicator, so this was a much-needed revision,” said Michael Moore, MD, Arilla Spence DeVault Professor of Otolaryngology–Head and Neck Surgery and medical director of the Indiana University Health Joe and Shelly Schwarz Cancer Center in Carmel. “By more accurately staging these cancers, we can better capture, from a prognosis standpoint, how these patients will do.”
Measuring Depth of Invasion
In the new AJCC staging system, the DOI is “measured first by finding the ‘horizon’ of the basement membrane of the adjacent squamous mucosa. A perpendicular ‘plumb line’ is established from the horizon to the deepest point of tumor invasion,” noted Cherie-Ann Nathan, MD, the Jack Pou Endowed Professor and chairman of the department of otolaryngology–head-neck surgery at Louisiana State University Health in Shreveport, La. Although studies have examined 3-, 4-, and 5-mm increments to determine lymph node metastasis and survival risk stratification, the experts involved in developing the AJCC8 settled on 5-mm increments, Dr. Nathan said (see Table 1).
By more accurately staging these cancers, we can better capture, from a prognosis standpoint, how these patients will do. —Michael Moore, MD
Most experts agree that the 2018 AJCC 8th edition staging system is more complex than its predecessor. “The purpose of cancer staging is to predict prognosis and therefore to guide appropriate treatment,” said Marita S. Teng, MD, professor and residency program director for the department of otolaryngology–head and neck surgery at the Icahn School of Medicine at Mount Sinai, New York City. “The 7th edition staging system had been criticized for years because of its suboptimal prognostication of oral cavity cancer.”
Many iterations of a redesigned staging system were considered, but ultimately, expert consensus settled on DOI and ENE. “The inclusion of DOI was an important change for oral cavity cancer,” agreed Daniel L. Faden, MD, assistant professor of otolaryngology–head and neck surgery at Harvard Medical School in Boston, Mass. “Previously, oral cavity cancers were staged by their size and the structures they invaded. However, DOI has become a well-established prognostic risk factor,” he said, with deeper tumors showing an increased risk of nodal metastases and decreased disease-specific survival. “Inclusion of DOI has led to an improved ability to predict survival.”
“AJCC8 reflects a more sophisticated view of the primary tumor so that the risk for recurrence and the risk for nodal metastasis is better refined,” said Erich M. Sturgis, MD, MPH, professor and vice-chair of clinical affairs in the department of otolaryngology–head and neck surgery and the Brown Foundation Endowed Chair of head, neck, and thyroid cancer at Baylor College of Medicine in Houston.
Differences in T-Category Between 7th and 8th AJCC Staging for Oral Cavity Cancers
| 7th Edition | 8th Edition |
|---|---|
| TX: Primary tumor cannot be assessed | TX: Primary tumor cannot be assessed |
| TO: No primary | -- |
| Tis: Carcinoma in situ | Tis: Carcinoma in situ |
| T1: Size ≤ 2 cm | T1: Size ≤ 2 cm and DOI ≤ 5 mm |
| T2: Size 2 - ≤ 4 cm | T2: Size ≤ 2 cm and DOI 5 - ≤ 10 mm or size 2 - ≤ 4 cm and DOI ≤ 10 mm |
| T3: Size > 4 cm or extension to lingual surface or epiglottis | T3: Size > 4 cm or any tumor DOI > 10 mm |
| T4 • T4a: Moderately advanced • T4b: Very advanced | T4 • T4a: Tumor invades adjacent structure only • T4b: Tumor invades masticator space, pterygoid plates, or skull base and/or encases the internal carotid artery |
DOI, depth of invasion
Adapted from AJCC Cancer Staging Manual. 8th ed. Springer International Publishing: American Joint Commission on Cancer; 2017.
In clinical practice, it may be difficult to accurately assess the DOI of an oral cavity cancer, which necessitates histologic evaluation. Prior to AJCC8, however, a T1 staged lesion that was thick (>10 mm) was staged the same as an intermediate (>5 mm and ≤10 mm) or thin (≤5 mm) lesion. “The new staging system does a better job of moving those thicker lesions out of T1 and into either T2 or T3, which follows how things have been done for many years for melanoma,” Dr. Sturgis said.
In a study by Weber and colleagues, occult nodal disease was found in 55 (26%) of the 212 patients. A DOI of 7.25 mm was most predictive for occult nodal disease and 8 mm for overall survival (OS) and disease-specific survival (DSS). The authors concluded that the optimal DOI cut-point for detection of occult nodal metastasis was 7.25 and 8 mm for OS and DSS, respectively, at five years (Head Neck. 2019;41:177-184).
The DOI may also be used as a cutoff for performing elective neck dissection in patients with early stage (T1-T2) oral cancer, although definitive studies need to be performed. Elective neck dissection has been shown to result in higher rates of OS and DSS compared with therapeutic neck dissection in patients with early-stage oral squamous cell cancer (Am J Surg. 1989;158:309-313; N Eng J Med. 2015;373:521-529).
In a nationwide British study (SEND), patients with localized stage T1/T2 disease who had their tumors resected with or without elective neck dissection were included. Two hundred fifty randomized and 346 observational patients from 27 hospitals were studied. Occult neck disease was found in 19.1% (T1) and 34.7% (T2) patients, respectively. The authors concluded that elective neck dissection was effective at prolonging survival and that it lowered recurrences for patients with T1/T2 small tumors. Patients who underwent neck dissection also experienced more facial/neck nerve damage; quality of life was largely unaffected (Br J Cancer. 2019;121:827-836).