 Thyroid cancer rates are up worldwide. Total thyroidectomy rates are declining.
Thyroid cancer rates are up worldwide. Total thyroidectomy rates are declining.
This apparent dichotomy is driven by two trends: increased diagnosis of thyroid cancer, largely due to increased availability and utilization of advanced imaging, and technological advances that enable physicians to treat thyroid cancers and nodules more precisely.
Over the past three decades, the incidence of thyroid cancer has “increased dramatically,” according to the American Thyroid Association (Clinical Thyroidology. https://tinyurl.com/2a6k996m). Thyroid cancer rates have tripled in the UK since the 1990s (Cancer Research UK. https://tinyurl.com/yefx6pmf); in the U.S., rates of thyroid cancer were growing faster than any other cancer until physicians adopted stricter diagnostic criteria in the mid-2010s (American Cancer Society. https://tinyurl.com/3h7vw6vx). Globally, thyroid cancer incidence is expected to increase by nearly 30%, and thyroid cancer-related mortality by 67%, by 2040 (Indian J Surg Oncol. doi:10.1007/s13193-021-01429-y).
In some parts of the world, likely overdiagnosis of thyroid cancer has led to an increase in the number of thyroidectomy procedures (Cancers (Basel).doi:10.3390/cancers15112931). In the U.S. and elsewhere, there’s been a “significant scaling back on how much thyroid surgery is done,” said David C. Shonka, Jr., MD, associate professor of otolaryngology–head and neck surgery at the University of Virginia School of Medicine in Charlottesville, as providers increasingly recognize the impact of surgical morbidity on patients’ quality of life.
“When I initially trained in thyroid surgery, surgeons were still using big incisions and removing the entire thyroid for small cancers,” Dr. Shonka said. “Now, we’re using smaller incisions and doing less surgery in general.”
Otolaryngologists today have more options than ever to safely manage thyroid cancers and nodules. Here is a look at the major advancements revolutionizing thyroid surgery.
New Approaches to Thyroid Surgery
One of the biggest shifts in the surgical management of thyroid disease has been the move toward performing as little surgery as possible. A “modest but significant increase” in lobectomy rates followed the release of the 2015 American Thyroid Association Differentiated Thyroid Cancer Guidelines update; however, the majority (82%) of patients with eligible papillary thyroid carcinoma were still treated with total thyroidectomy (Endocr Oncol.doi:10.1530/EO-22-0095). A retrospective study of surgical management practices at high-volume centers noted a significant shift in management from 2010 to 2018—the percentage of patients with likely malignant thyroid nodules and no clinical evidence of further diseases treated with total thyroidectomy plus prophylactic neck dissection decreased from 50% to 10%. The proportion of patients with likely malignant modules treated with thyroid lobectomy increased from 2% to 19%, and diagnostic thyroidectomies in patients with cytologically indeterminate nodules decreased from 67% to 35% (Thyroid. doi:10.1089/thy.2019.0783).
 The move toward less surgery has likely been “a big benefit to patients,” Dr. Shonka said, as morbidity related to thyroid removal can significantly affect patients’ quality of life for decades.
The move toward less surgery has likely been “a big benefit to patients,” Dr. Shonka said, as morbidity related to thyroid removal can significantly affect patients’ quality of life for decades.
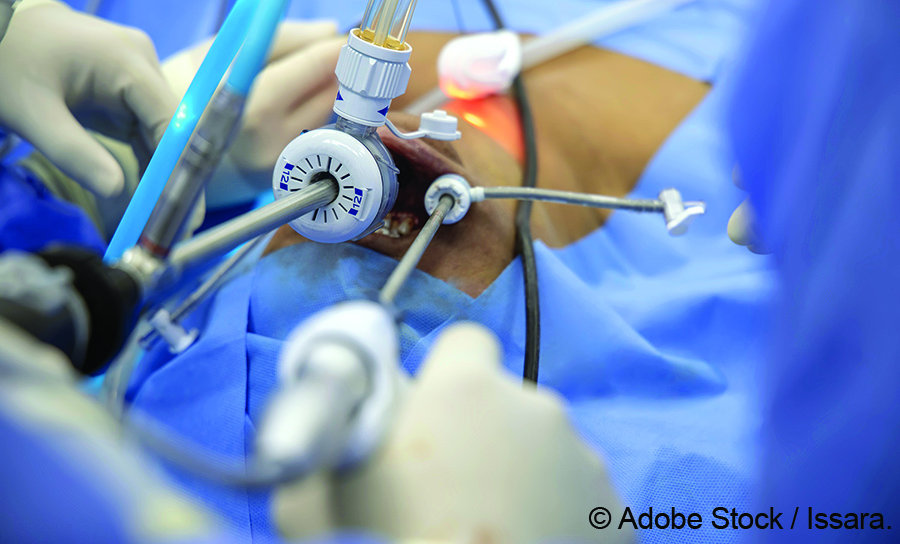
Patients who need thyroid surgery but wish to avoid a scar on their neck can now choose remote-access thyroid surgery, at least at some institutions. Options include the trans-axillary approach, the bilateral axilla-breast approach, and natural orifice (transoral) surgery.
Although these methods have been described as minimally invasive techniques (Cancers (Basel). doi:10.3390/cancers15112931), remote access thyroid surgeries are complex and typically take significantly longer than traditional thyroid surgery. Costs may be higher due to the cost of equipment and increased operative time. Additional complications—such as brachial plexus injury—can occur, depending on the approach (Indian J Surg Oncol. doi.org/10.1007/s13193-021-01364-y).
We don’t potentially put the good nerve at risk; we can stage the other side if we are concerned that we have a nerve injury on one side, and come back another day. —Vaninder Dhillon, MD
Robotic transoral thyroid surgery is not commonly done in the U.S. Dr. Shonka doesn’t perform it; neither does Vaninder Dhillon, MD, assistant professor of otolaryngology–head and neck surgery at Johns Hopkins University School of Medicine and Johns Hopkins Otolaryngology–Head and Neck Surgery in Bethesda, Md.
“I trained in a place where a lot of transoral surgery was done, but I have not adopted it into my practice,” Dr. Dhillon said. “But I do offer it to my patients because some of my colleagues do it. If a scar is a reason a patient doesn’t want to do surgery, I encourage them to meet with one of my colleagues, because a scar can be avoided.”
Although transoral surgery has been around for some time, it seems to have had a fairly limited impact in the U.S. and has not been incorporated in some major cancer centers, according to Gregory W. Randolph, MD, professor of otolaryngology–head and neck surgery and the Claire and John Bertucci Endowed Chair in Thyroid Surgical Oncology at Harvard Medical School in Boston.
Intra-Operative Nerve Monitoring
In contrast, nerve monitoring is a transformative technology that is now routinely applied in thyroid and parathyroid surgery, with a 2022 editorial in the Journal of Clinical Medicine calling it “the gold standard to reduce post-thyroidectomy voice complications” (J Clin Med.doi:10.3390/jcm11237233).
Much as a Doppler allows vascular surgeons to assess the movement of blood through a vessel, intra-operative nerve monitoring (IONM) allows physicians to assess the function of crucial nerves—typically, the recurrent laryngeal nerve (RLN)—during thyroid surgery.
“You can test, in real-time, the integrity of the recurrent laryngeal nerves during the operation,” Dr. Shonka said. Because the technology measures the electrical activity of the nerve, physicians can detect negative changes and adapt surgery to prevent additional harm. So, if IONM reveals impaired function of the right RLN, the surgeon can stage and delay surgery on the other side until a future date.
“We don’t potentially put the good nerve at risk; we can stage the other side if we are concerned that we have a nerve injury on one side, and come back another day,” Dr. Dhillon said.
Research to date suggests that IONM decreases morbidity and improves patient outcomes and quality of life. A review of nearly 5,500 cases found that when surgeons routinely used nerve monitoring during thyroid cancer surgery, the incidence of vocal cord dysfunction was 2.4% in the short term and 2.2% in the long term, compared to 4.4% and 3.7%, respectively. Routine use of IONM was independently associated with a decreased risk of short- and long-term vocal cord dysfunction, a lower risk of post-op hypoparathyroidism, and a higher likelihood of same-day discharge (BMC Surg. doi:10.1186/s12893-023-02122-3).
Like every technology, the utility of IONM depends, in part, on the skill and knowledge of the one using it. Intermittent nerve monitoring, for instance, is more useful if it’s done frequently throughout surgery, as opposed to sporadically. (Continuous nerve monitoring systems are available, but “much less utilized,” Dr. Randolph and others said.) Real-world use of IONM is still selective. According to the 2014 to 2021 Collaborative Endocrine Surgery Quality Improvement Program thyroidectomy and parathyroidectomy datasets, surgeons are more likely to use IONM during thyroid surgery than parathyroid surgery. Those who routinely use IONM during thyroidectomy are more likely to use the technology during parathyroidectomies, but there is a 43% decrease in the routine use of IONM between thyroidectomy and parathyroidectomy (Surgery. doi:10.1016/j.surg.2023.11.024).
Increasingly, surgeons are using IONM to monitor the external branch of the superior laryngeal nerve (EBSLN) during surgery as well. The EBSLN innervates the cricothyroid muscle, which impacts vocal pitch and projection, so proper functioning of the nerve is particularly important to singers and other people who use their voices professionally. Because damage to the EBSLN can cause significant morbidity, Amanda L. Silver Karcioglu, MD, clinical assistant professor at the University of Chicago Pritzker School of Medicine, monitors it routinely.
“When I was in residency, it was not a nerve we routinely monitored,” she said. “Now that we can, I monitor it in every case when I’m working near the superior pole of the thyroid.” Doing so doesn’t require any additional tools, as the same technology that’s used to monitor the RLN can be used on the EBSLN.
EBSLN monitoring isn’t yet widespread. Just 11% of surveyed Spanish endocrine surgeons report stimulation of EBLSN during all thyroidectomies, even though 78% monitor the RLN during all thyroidectomies (Sci Rep. doi:10.1038/s41598-024-68230-z). It is unknown how common EBSLN monitoring is in the U.S.
Targeted application of IONM during thyroid and parathyroid surgeries, including increased use of EBSLN monitoring, may further decrease surgical morbidity and enhance patients’ quality of life.
“Nerve monitoring overall is now widely disseminated, but there’s still a long way to go to make sure that people are getting all they can out of nerve monitoring,” Dr. Randolph said.
Parathyroid Identification
Hypocalcemia due to inadvertent parathyroid damage is one of the most common complications of thyroidectomy. Research from Sweden and elsewhere suggests that the risk of permanent hypocalcemia after total thyroidectomy is higher than previously understood—and may be underestimated (Br J Surg. doi:10.1093/bjs/znad366; Ann Surg. 2021. doi: 10.1097/SLA.0000000000003800). Research has also shown widespread effects of hypocalcemia on the body and patients’ quality of life. A 2023 meta-analysis of 81 studies found that hypoparathyroidism is associated with an increased risk of cataracts (with prevalence rates ranging from 27% to 55%), neuropsychiatric sequelae (including depression and seizures), and cardiac arrhythmias (Ann Thyroid. doi:10.21037/aot-22-10). Other long-term impacts of hypocalcemia include an increased risk of renal insufficiency and increased risk of any malignancy; patients with cardiovascular disease at the time of thyroidectomy also have an increased risk of cardiovascular events during follow-up (Surgery. doi: 10.1016/j.surg.2019.06.056).
“The impact on patients’ lives is actually quite substantial,” Dr. Karcioglu said.
One way to decrease the risk of hypoparathyroidism (and associated untoward effects) is to avoid unintentional removal of or damage to the parathyroids. The U.S. Food and Drug Administration granted clearance to two different parathyroid detection systems in 2018: one, probe based; and the other, camera based. Both are based on the discovery that parathyroid glands autofluoresce under near-infrared light (JAMA Otolaryngol Head Neck Surg. doi:10.1001/jamaoto.2022.4421).
“This is another example of a technology that is additive to what a surgeon’s eyes and technique provide and helps with definitive identification of parathyroid tissue,” Dr. Randolph said.
The probe-based detection system is analogous to the technology used for IONM. “If you’re used to using a probe for nerve monitoring, this is very simple and easy,” Dr. Karcioglu said. “You simply touch the tissue of interest with the probe and use a foot pedal to activate the probe and get a detection ratio, and you can do that as many times as you want during surgery.”
Because the parathyroids autofluoresce even after removal from the body, surgeons can use technology to check surgically excised matter for parathyroid tissue. “If they see a bright spot in the tissue, they may be able to reimplant parathyroid glands they’ve inadvertently removed,” Dr. Shonka said.
You can test, in real time, the integrity of the recurrent laryngeal nerves during the operation. — David C. Shonka, Jr., MD
Of course, the fact that the glands autofluoresce even when devascularized is one shortcoming of most existing parathyroid detection systems. The current systems are not able to determine if identified parathyroid glands will be functional after surgery. Indocyanine green (ICG) can be used to assess the function of the parathyroid glands during surgery but requires extra steps and limits the use of near-infrared autofluorescence following administration (In Vivo. doi:10.21873/invivo.11741).
At present, “there is more data supporting the utility of autofluorescence to identify parathyroids during thyroid and parathyroid surgery, at an earlier stage of its introduction, as compared to nerve monitoring,” Dr. Randolph said. “So, I would expect that autofluorescence with cameras and probes will be routinely applied in an even shorter time than it took for nerve monitoring to be widely adopted.”
Cost, however, may be a barrier. “In this cost-conscious healthcare environment, it’s sometimes hard to get hospital systems to buy equipment that cannot be directly reimbursed,” Dr. Karcioglu said.
Nonsurgical Treatment
Advances in the nonsurgical treatment of thyroid conditions are also contributing to a decrease in thyroid surgery. Active surveillance is now a “reasonable treatment option for some very small thyroid cancers in the appropriate clinical setting,” Dr. Shonka said. Energy-based ablation techniques, including laser, radiofrequency, and microwave, can be used to treat benign thyroid nodules and some small cancers, minimizing the need for thyroid surgeries. And, the rapid development of targeted therapies to treat thyroid cancer now offers potential opportunities for cures in cases that would have previously been deemed incurable.
“Multiple clinical trials are currently looking into targeted systemic therapy followed by surgery,” Dr. Shonka said. Evidence to date suggests that neoadjuvant therapy may shrink tumors and perhaps allow physicians to perform less surgery, with improved morbidity and better oncologic outcomes.
Each of these innovations is changing the landscape of thyroid surgery. Right now, otolaryngologists must master and adopt multiple tools and techniques to harness the power of these advances. In the not-so-distant future, these innovations may be combined into an easier-to-use interface, such as a technology-packed “helmet” or “Google Glass-type device,” Dr. Randoph said.
“Right now, we have individual disparate technologies all extending into the surgical space. They’re like individual planks to cross the valley and get us to where we need to be. They need to be melded into one multifunctional interface that will form a steel bridge to get us to the other side,” Dr. Randolph said. “And I think that will happen.”
Jennifer Fink is a freelance medical writer based in Wisconsin.
New Focused Practice Designation: Adult Complex Thyroid and Parathyroid Surgery
Otolaryngologists who would like to achieve formal recognition of their proficiency in the surgical management of thyroid disease can now choose to pursue a Focused Practice Designation (FPD) in Adult Complex Thyroid and Parathyroid Surgery (ACTPS).
Developed jointly by the American Board of Surgery and the American Board of Otolaryngology-Head and Neck Surgery, the new FPD (The American Board of Surgery. https://tinyurl.com/mkrk9sre) reflects the continuing move toward hyper-specialization and is intended to recognize physicians who devote a significant part of their practice to thyroid surgery.
“It’s an opportunity to designate that a given surgeon has a focus in this area that is backed up by certain volume numbers that have quality implications,” said Gregory W. Randolph, MD, professor of otolaryngology–head and neck surgery and the Claire and John Bertucci Endowed Chair in Thyroid Surgical Oncology at Harvard Medical School in Boston.
Eligible, non-fellowship-trained candidates must have performed a total of 120 or more (including 24 complex) thyroid/parathyroid cases over three consecutive years. Candidates who have completed a fellowship providing thyroid/parathyroid case experience must provide evidence of at least 80 cases (including 16 complex) within their first two years of practice following fellowship completion (The American Board of Surgery. https://tinyurl.com/mw9tt3m8).
I think it remains to be seen what ultimate value it will have, particularly for patients.” —Amanda L. Silver Karcioglu, MD
The benefits of ACTPS FPD are yet to be demonstrated. “One would think that perhaps patients, referring doctors, and even hospitals may, at some point, consider the focus practice designation as a badge of added quality due to focus and volume,” Dr. Randoph said.
“I think it remains to be seen what ultimate value it will have, particularly for patients,” said Amanda L. Silver Karcioglu, MD, clinical assistant professor at the University of Chicago Pritzker School of Medicine.
Applications for the first ACTPS FPD examination—an approximately 150-question multiple-choice computerized test—are currently open. The exam will be administered at secure testing centers from April 7-9, 2025.
