 TRIO Best Practice articles are brief, structured reviews designed to provide the busy clinician with a handy outline and reference for day-to-day clinical decision making. The ENTtoday summaries below include the Background and Best Practice sections of the original article. To view the complete Laryngoscope articles free of charge, visit Laryngoscope.
TRIO Best Practice articles are brief, structured reviews designed to provide the busy clinician with a handy outline and reference for day-to-day clinical decision making. The ENTtoday summaries below include the Background and Best Practice sections of the original article. To view the complete Laryngoscope articles free of charge, visit Laryngoscope.
Explore This Issue
October 2017Background
Medialization procedures reliably improve glottic insufficiency symptoms, such as dysphonia and aspiration, by altering the vocal fold position. Laryngeal framework surgery (LFS), most commonly medialization laryngoplasty (also known as type I thyroplasty), offers a durable treatment option for glottic insufficiency. The vocal fold is medialized by insertion of an implant through the thyroid cartilage into the paraglottic space. Several implant materials are confirmed to be safe and to have excellent voice outcome: Silastic, polytetrafluoroethylene ribbon, titanium, and hydroxylapatite implants.
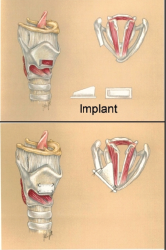
Medialization laryngoplasty procedure.
External beam radiation is common employed in the treatment of head and neck cancer. Patients who recovered from head and neck cancer often seek solutions for side effects caused by the treatment. Many patients with radiation history may experience concurrent glottic insufficiency that aggravates symptoms of dysphonia. Vagal or recurrent laryngeal nerve injury induced by surgery or radiation, vocal fold atrophy, vocal fold tissue defects, and cricoarytenoid fixation can contribute to glottic insufficiency. Many laryngeal framework surgeons consider previous radiation to the neck and larynx a relative contraindication for LFS. Generally, surgery in a previously radiated surgical field is challenging, time consuming, and poses a higher rate of complications. Radiation alters tissue vascularity and promotes fibrosis, which may result in slow recovery, uncontrolled postoperative infections, chondritis/chondronecrosis, ischemic damage to the nearby poorly vascularized mucosa, and implant extrusion.
The arguments against LFS performed in the radiated field are generally based on individual practice, experience from other head and neck surgeries performed in the radiated neck, and analogies with other surgical disciplines. However, there are no published objective studies to support these arguments. Nevertheless, evidence to support any surgical treatment for dysphonia in radiated patients is limited as well. Recent evidence sheds more light on the safety of LFS in the radiated larynx.
Best Practice
LFS in radiated patients can be considered to be safe and effective. However, to optimize safety and outcomes, careful patient selection should be practiced with respect to indication, patient’s needs, degree of laryngeal fixation, soft tissue scarring, and radiation field and dosage. Discussing possible complications and realistic expectations is particularly important for LFS in irradiated patients. Furthermore, due to challenging surgical conditions and possible increased complication rate, LFS in radiated patients should preferably be performed by experienced surgeons. Overall, with proper patient selection, LFS in radiated patients appears to be safe with reasonable rates of complications (Laryngoscope. 2017;127: 778–780).