 Imaging of parathyroid adenomas, efficacy of functional rhinoplasty, an emerging therapy for recurrent respiratory papillomatosis, betahistine for Ménière’s disease, and the state of surgical training were all tackled by a panel of experts at the Triological Society Combined Sections Meeting in a series of Best Practice talks—condensed presentations on practical clinical considerations based on available evidence.
Imaging of parathyroid adenomas, efficacy of functional rhinoplasty, an emerging therapy for recurrent respiratory papillomatosis, betahistine for Ménière’s disease, and the state of surgical training were all tackled by a panel of experts at the Triological Society Combined Sections Meeting in a series of Best Practice talks—condensed presentations on practical clinical considerations based on available evidence.
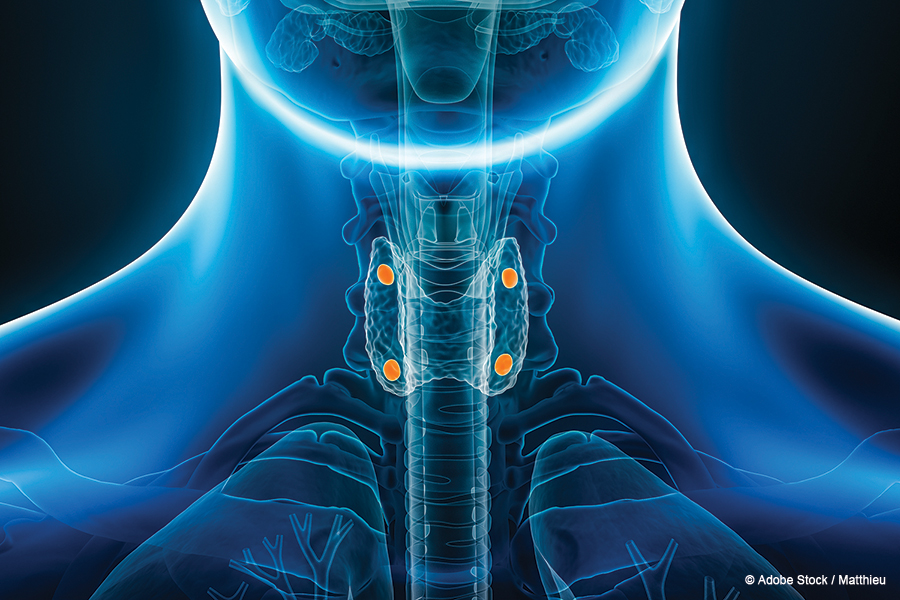
Parathyroid Adenoma Imaging
All of the most common imaging modalities for parathyroid adenomas have merit, depending on the situation and surgeon comfort, said Samir Khariwala, MD, MS, chair of otolaryngology–head and neck surgery at the University of Minnesota, Minneapolis, in one presentation.
Perhaps [MRI] is an adjunct—not necessarily superior, but a different modality—that can be used when the adenoma is not identified on sestamibi.” — Samir Khariwala, MD, MS
These parathyroid adenomas can be very difficult cases depending on the type. “As any surgeon who does this kind of procedure knows, localized [and] non-localized adenomas … require significantly different planning,” Dr. Khariwala said. “A localized adenoma is a really quick operation; a non-localized adenoma can be sometimes even soul-crushing.”
When parathyroid adenomas are identified accurately, the cost, the length of surgery, and the need for additional procedures are reduced, “so obviously we want to try to identify them as accurately as possible,” he said.
Several modalities are available for adenoma detection, and the one that’s chosen may vary by the surgeon and the patient.
One study evaluated magnetic resonance imaging (MRI) alone and as an adjunct to sestamibi scanning. Researchers found that MRI detected 16 of 25 adenomas, compared with 18 of 25 for sestamibi, but it also found four of seven that were not identified on sestamibi.
“So perhaps [MRI] is an adjunct—not necessarily superior, but a different modality—that can be used when the adenoma is not identified on sestamibi,” he said.
A 2016 paper on guidelines by the American Association of Endocrine Surgeons suggested that the imaging modality for adenomas should be chosen by the experienced surgeon, that ultrasound is the most cost-effective, and that MRI and venous sampling could be considered when there is a challenging component to the case, such as a re-do or a non-localized adenoma (JAMA Surg. 2016;151:959–968).
A meta-analysis including 43 studies found that ultrasound and sestamibi showed similar efficacy, and that 4D-computed tomography (CT), a newer modality, may be superior, but too few studies exist to make a conclusion, Dr. Khariwala said (Ann Surg Oncol. 2012;19:577–583).
Another study, in 2019, compared fine needle aspiration (FNA) with parathyroid hormone (PTH) washout to ultrasound and sestamibi and found that sensitivity, specificity, and positive and negative predictive values were all best for FNA
(J Endocrinol Diabetes. 2019;6:1–6).
An economic analysis found that the imaging modalities were fairly similar in cost, ranging from about $6,000 to $6,400 (Ann Surg Oncol. 2012;19:4202–4209).
“You don’t really see a lot of cost difference based on what imaging modality you use, so the cost is coming from the surgery and anesthesia, which all of these patients are eventually going to get,” Dr. Khariwala said.
“All four modalities that are commonly studied in the literature [i.e., MRI, CT, ultrasound, and sestamibi] offer efficacy in specific situations and specific hands,” he said. “MRI may be a useful adjunct in challenging cases. … Things that are lower in the chest are going to be hard to visualize with ultrasound, for example, so cross-sectional imaging is a little more useful in those cases.”
Functional Rhinoplasty
Stephen Park, MD, chair of otolaryngology–head and neck surgery at the University of Virginia in Charlottesville, said that functional rhinoplasty has repeatedly been found to be effective, but choosing the right graft is central to success. The options are many—spreader grafts, butterfly grafts, flaring sutures, suspension sutures, lateral wall batten grafts, lateral crural strut grafts, alar rim grafts, and office-based procedures.
One paper—a 25-year systematic review by researchers at the University of Wisconsin in Madison—included 44 papers, most of which were case series, and found that functional rhinoplasty was effective in all of them, ranging from 65–100% improvement (Otolaryngol Head Neck Surg. 2008;139:10–20). But Dr. Park cautioned that the outcomes were reported very differently—some subjectively, some with the visual analog scale, and some with questionnaires that were only occasionally validated.
Another systematic review and meta-analysis looked at 16 studies that used only Nasal Obstruction and Septoplasty Effectiveness (NOSE) scores to assess the procedures (Otolaryngol Head Neck Surg. 2017;156:809–815). They found an improvement in all of the studies, from 43 to 50 points out of 100. But there was no distinction between etiology, graft, and technique types, Dr. Park noted.
Another systematic review and meta-analysis found no difference between spreader grafts and auto-spreader grafts but with varying methods and outcome measures. That analysis included 52 studies, 17 of which used NOSE scores for their assessment (Aesthetic Plast Surg. 2022;46:1741–1759).
And another study—a prospective case series with 704 patients—compared lateral crural strut grafts with alar rim grafts and found improvement for all and no difference between the two approaches, Dr. Park said (Facial Plast Surg Aesthet Med. 2022;24:240–246).
“Ideally, you would randomize them—and realistically and practically speaking, that’s never going to happen,” he said.
The judgment of the surgeon is going to play a major role in the outcome of these procedures, Dr. Park said.
“The way I interpret all of these is that these operations work, but the key part of this is actually matching the precise anatomic etiology of their pathology with the specific graft or technique,” he said. “You have to be very specific and accurate in identifying where the pathology is, and that would lead you to the proper technique. That skill set is pivotal and learned in clinic, seeing the patient pre-operatively.”
Recurrent Respiratory Papillomatosis
Craig Derkay, MD, professor of otolaryngology at Eastern Virginia Medical School in Norfolk, said that growing evidence indicates that recurrent respiratory papillomatosis (RRP) is destined to become mostly a disease treated medically rather than one addressed mainly with surgery.
The monoclonal antibody bevacizumab binds to and inhibits vascular endothelial growth factor (VEGF), which is expressed on the endothelium of papillomas, inhibiting their blood supply and, thereby, blocking angiogenesis. It’s available as an intralesional injection or systemically and now is available in a biosimilar form.
It has been approved by the U.S. Food and Drug Administration as a first-line treatment for advanced and metastatic colorectal and cervical cancers, among other cancers, as well as for diabetic retinopathy and age-related macular degeneration. Otolaryngologists have used it off-label for the treatment of neurofibromatosis type 2 and RRP.
Promising results have been seen for the use of bevacizumab for RRP in case series from around the world. A 2021 systematic review that included 12 studies found systemic bevacizumab to be safe and effective, with reduced need for surgery (Laryngoscope. 2021;131:1138–1146). An international consensus statement from 70 experts in 12 countries—led in part by Dr. Derkay—found that systemic bevacizumab was a highly promising option (Laryngoscope. 2021;131:E1941–E1949).
“Our consensus is that it’s effective both early and late in the disease process,” said Dr. Derkay. “There was no difference in terms of response rates between those patients who were started early on in their papilloma diagnosis versus those who had already had dozens of operations.” The drug was effective in the larynx, as well for tracheal disease and pulmonary disease, he said, adding that it’s effective in both adults and children.
Systemic bevacizumab seems poised to succeed where many other therapies have not, said Dr. Derkay.
“We’ve had many false hopes in the last several decades with interferon and indole-3-carbinol and cidofovir,” he said. “I could give you a dozen names of adjuvant therapies that have been tried, but bevacizumab looks like it’s really going to be our savior here.”
Systemic use has been found to be superior to the intralesional form, which has been found to be no more effective than intralesional cidofovir.
The consensus statement recommends starting with an initial loading dose of 10 mg/kg after debridement of all visual papillomas that are reachable, with repeat dosing at three-week intervals, initially. Clinicians should try to stretch out those intervals to try to prevent regrowth and prevent symptoms. Renal and hepatic functions need to be monitored, and those with pulmonary disease should be monitored through CT scans, he said.
The drug is not a cure for RRP but seems to be a good option, especially compared with surgery. Two DNA vaccines, with a cure as the goal, are being assessed in phase 3 trials, he said.
Ménière’s Disease
In another presentation, Gauri Mankekar, MD, PhD, assistant professor of otolaryngology–head and neck surgery at Louisiana State University Health in Shreveport, discussed the effectiveness of betahistine, a histamine analog thought to work by increasing blood flow to the cochlea, for Ménière’s disease.
The drug is not currently approved by the FDA in the U.S., but it can be obtained from compounding pharmacies and is prescribed by U.S. physicians.
Overall, there is not much evidence to show that it’s effective, Dr. Mankekar said.
A 2001 Cochrane review that included seven randomized controlled trials with a total of 243 patients and a follow-up time of up to 40 weeks, found no evidence that the therapy was either effective or ineffective. But only one trial used the American Academy of Otolaryngology-Head and Neck Surgery guidelines for diagnosing Ménière’s (Cochrane Database Syst Rev. 2001;2001: CD001873).
Another Cochrane review, in 2016, with 17 randomized controlled trials and 1,025 patients with vertigo of different causes, had a follow-up of up to three months and found only low-quality evidence that suggested a positive effect of betahistine on vertigo symptoms, but found that it is well tolerated, with a low risk for adverse events (Cochrane Database Syst Rev. 2016;2016:CD010696). Reviewers found a high level of heterogeneity among the trials.
Other reviews and analyses have been similarly short on evidence of efficacy (Acta Otolaryngol. 2020;140:845–853).
“There is an absence of high-quality data to demonstrate the efficacy of betahistine in the treatment of Ménière’s disease,” Dr. Mankekar said. “Despite all these mixed results, [betahistine] remains very popular because it has a very low-risk profile. Large-scale randomized trials using standard diagnostic criteria, standard dosing regimens and formulations, long-term follow-ups, and using standardized outcome testing may tell us more about the efficacy of betahistine in Ménière’s disease.”
Physicians commenting after the talk said they have experience with the drug helping to spare patients from surgery, and that physicians need to consider the stage of the disease when choosing treatment.
“It’s nice to compare to control groups and other things, but we know Ménière’s disease has quite a spectrum, and part of that is what the timing is of the disorder and what we’re treating during what part of that disorder,” said Fred Telischi, MD, MEE, chair of otolaryngology at the University of Miami Miller School of Medicine.
Modernizing Surgical Training
Mona Abaza, MD, MS, professor of otolaryngology—head and neck surgery at the University of Colorado School of Medicine in Aurora, said the evidence suggests that surgical training would benefit from moving beyond the approach of one mentor with several mentees watching and learning and progressing gradually toward autonomy, a technique introduced in 1904.
“Many can claim that, other than 120 years passing, not a whole lot has changed,” Dr. Abaza said.
A proven approach is the more deliberate briefing, interoperative teaching, and debriefing (BID) model, which includes the briefings that surgeons are used to now but within a teaching model. In this model, the mentor asks what the mentee would like to learn during the procedure, includes instruction to that end during the procedure, and discusses afterward what was done well and what needs improvement.
This model has been studied in every subspecialty, including otolaryngology, Dr. Abaza said.
Mentors might think they engage enough with their mentees, but that might not actually be the case, she said.
“While we all think we intuitively do it, the data suggest that residents only feel they’re receiving feedback 18% of the time,” she said.
A potentially useful assessment tool is the Ottawa Surgical Competency Operating Room Evaluation (O-SCORE), commonly used across Canada, which assesses pre-procedure planning, knowledge of specific steps, technical performance, communication, and other aspects of surgery.
Dr. Abaza said she thinks it would be beneficial to the field for all institutions to use a single model.
“I do think, particularly because we’re a smaller surgical specialty than a lot of them,” she said, “that it can make sense for us to look at something that’s more global that fits all of us, so that apples can be compared to apples, and not apples to oranges.”
Thomas R. Collins is a freelance medical writer based in Florida.