
Patient undergoing sleep endoscopy.
© Voisin / Phanie / Science Source.com
Deciding how to evaluate and treat hypopharyngeal obstructive sleep apnea (OSA) is often not a straightforward proposition, but many options exist for getting the best results for patients, according to a panel of experts who convened at the annual meeting of the American Academy of Otolaryngology-Head and Neck Surgery.
The wide-ranging panel covered the need for better ways to identify airway obstruction sites, radiofrequency tongue reduction, transoral robotic surgery, a system for grading lingual tonsil hypertrophy, endoscopic coblator open tongue base resection, epiglottic collapse and laryngomalacia, and the role of skeletal surgery.
Identifying the Obstruction Site
Eric Kezirian, MD, MPH, professor of sleep medicine in the department of otolaryngology-head and neck surgery at the University of Southern California in Los Angeles, stressed the importance of identifying the site or sites of obstruction. Several studies have cited the need for better ways to do this (Cochrane Database Syst Rev. 2000;(2):CD001004; 2005;(4):CD001004).
“Although sleep apnea is not entirely related to anatomy, when it comes to surgery, we are treating the anatomy. We want to make the most accurate determination of the anatomical issues and treat patients individually,” he said.
OSA severity as a sign of site obstruction—the idea that mild-to-moderate OSA is likely a result of collapse at the palate level and that moderate-to-severe sleep apnea likely includes some component of hypopharyngeal collapse—is inaccurate and is not supported by the evidence. Also, the Friedman system, which involves considering relative tongue size, tonsil size, and body mass index, is not sufficient for guiding surgical decisions by itself in the majority of patients, he added.
Drug-induced sleep endoscopy (DISE), designed to visualize the pattern of obstruction by reproducing the patterns seen on a sleep study, is becoming more commonly used; however, it is not a simple procedure and does require some time in the operating room or procedure suite. Dr. Kezirian is leading an international collaborative study to better tease out how DISE findings are associated with outcomes of sleep apnea surgery.
By improving the assessment, he said, “we may be able to develop targeted, more effective treatment of sleep apnea with surgery, and probably oral appliances as well.
Radiofrequency Tongue Reduction
Edward Weaver, MD, MPH, chief of sleep surgery at the University of Washington and co-director of the UW Medicine Sleep Center in Seattle, said radiofrequency surgery under local anesthesia over a series of sessions to reduce tongue size can be a good, minimally invasive option for some patients. But, it’s important for patients to have realistic expectations, and those with severe problems, such as a very high apnea-hypopnea index (AHI), a huge tongue, and a floppy palate—wouldn’t be good candidates.
Results have been found to be good for mild to moderate sleep apnea, with more sessions translating to greater success. But patients still showed residual apnea (Otolaryngol Head Neck Surg. 2003;128:848-861). Tongue-channeling, which is not heat-based and is performed over one or two sessions, involves the shrinkage of deep musculature and connective tissue. Large reductions in AHI and sleepiness have been seen in a case series with this approach (J Clin Sleep Med. 2013;9:117-124). “It’s typically, in my mind, an adjunctive treatment,” Dr. Weaver said.
“I use radiofrequency [tongue reduction] for patients who have primary complaint of snoring and very mild sleep apnea,” said panel moderator Michael Friedman, MD, professor of otolaryngology-head and neck surgery at Rush University Medical Center in Chicago and medical director for Chicago ENT.
TORS for Tongue Reduction
Erica Thaler, MD, professor of otolaryngology-head and neck surgery at the University of Pennsylvania in Philadelphia, said she started using transoral robotic surgery (TORS) for base of tongue reduction a few years ago. “It has evolved to be my way of most often dealing with challenging tissue at the base of the tongue and dealing with hypopharyngeal obstruction,” she said. Her outcome data show that, among patients who had undergone no prior surgery, AHI was reduced by 67%.
We want to make the most accurate determination of the anatomical issues and treat patients individually. —Eric Kezirian, MD, MPH
Dr. Thaler said that she has no hard cap on body mass index for TORS candidates and added that a patient’s physiognomy is an important consideration: If a patient has more body mass below the neck, he or she could be a candidate despite having a high BMI, and vice versa. “It’s not a trivial procedure of getting the patient through postoperative pain management,” she said. “It’s probably the toughest part of this for me, but it’s great surgery to handle this area.”
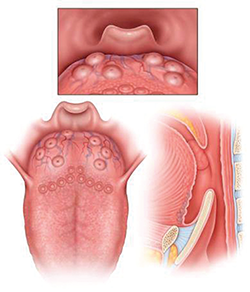
LTH Grade 1: Lymphoid tissue scattered over tongue, does not cover entire surface of tongue base.

LTH Grade 2: Lymphoid tissue covering entire tongue base, limited vertical thickness.
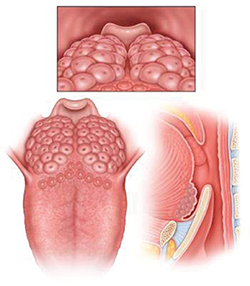
LTH Grade 3: Lymphoid tissue covering entire tongue base, vertical thickness between 5-10 mm, approximately 25-75% of height of epiglottis.
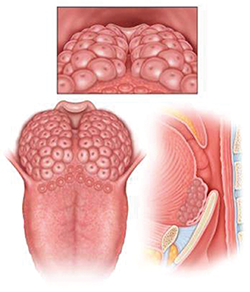
LTH Grade 4: Lymphoid tissue covering entire tongue base, vertical thickness approximately 1 cm, rises above tip of epiglottis.
Rating Lingual Tonsillar Hypertrophy
Dr. Friedman introduced a new way of systematically rating the degree of lingual tonsillar hypertrophy (see figure above):
- Grade 1: Lymphoid tissue scattered over the tongue;
- Grade 2: Lymphoid tissue covering the tongue but with limited vertical thickness;
- Grade 3: Between 25% and 75% of the height of the epiglottis; and
- Grade 4: Vertical thickness rising above the tip of the epiglottis.
“If we are going to study the efficacy of lingual tonsillectomy, we have to have a common language,” he said. “We can’t have one study doing Grade 4 tonsils and one study doing Grade 1.”
Endoscopic Coblation Open Tongue Base Resection
Hsin-Ching Lin, MD, associate professor of otolaryngology at Chang Gung University and vice chair of otolaryngology at Kaohsiung Chang Gung Memorial Hospital in Kaohsiung, Taiwan, described his center’s success with endoscopic coblation open tongue base resection, a procedure geared toward those who have moderate-to-severe OSA, have a large base of tongue on exam, and have failed continuous positive airway pressure (CPAP) treatment.
At his center, significant improvement in sleepiness, snoring, AHI, and oxygen levels have been seen, Dr. Lin said. Among 234 patients, AHI fell from an average of 44.9 prior to surgery to 28.2 afterward. Scores on the visual analog scale for snoring fell from 9.87 to 4.07 (p
“Endoscopic coblator base of tongue reduction should have significant potential in the treatment of selected patients with OSA,” he said.
Epiglottal Collapse and Laryngomalacia
Epiglottal collapse and laryngomalacia, more common in children than in adults, frequently involves a neuromuscular issue, said Kathleen Yaremchuk, MD, chair of otolaryngology-head and neck surgery at Henry Ford Hospital in Detroit. “There is a degree of neuropathy in these patients that occurs, and I always say you can’t trust the sleep apnea patient to breathe,” she said. “They don’t breathe when they’re asleep, and even when they’re awake there are abnormalities present.”
Beyond obstruction, part of it is the mechanical load and the compensatory neuromuscular responses, she added. CPAP is often ineffective in these patients because as soon as the machine is turned on with positive pressure, the epiglottis is pushed inferiorly and blocks the airway. The patient feels as if she is being suffocated.
Partial epiglottectomy has been shown to be an effective treatment. Dr. Yaremchuk referred to a study in which 27 adults with OSA and 12 infants with stridor were treated with this approach. OSA improved in 85% of the cases, and all of the infants improved (Ann Otol Rhinol Laryngol. 2000;109 (12 Pt 1):1140-1145).
Skeletal Surgery
Maxillomandibular advancement (MMA) has consistently shown the highest rates of surgical success for patients with OSA who cannot tolerate CPAP, said Stanley Liu, MD, DDS, assistant professor of otolaryngology at Stanford University. The surgery involves advancement and rotation of the mandible to increase pharyngeal muscle tension (Med Clin North Am. 2010;94:479-515).
“MMA’s efficacy may be due to decreased collapsibility of the upper airway muscles, or due to reduced negative pressure with stable air flow,” Dr. Liu said. “It’s probably a little bit of both.”
“What I found via drug-induced sedation endoscopy is that MMA reliably addresses complete collapse of the lateral pharyngeal wall and the soft palate,” he said. “The effect at the tongue level is less predictable. Relapse also tends to occur at the tongue level. With the advent of upper airway stimulation [hypoglossal nerve stimulation] to help me address where the MMA falls short, the playbook is now more complete than ever for patients seeking surgical solutions for OSA.”
The improvements result from enhancement of the tension of the pharyngeal wall, which increases airway stability, and stabilization of the velum, which lessens the collapse. In fact, he said, patients with concentric collapse of the soft palate and a “severe lateral pharyngeal wall collapse” should probably move straight to an MMA procedure. Afterward, these patients can still go back for other procedures, such as tongue base reduction.
“The playbook is wide open,” he added. “It’s just how we decide that treatment-planning tree.”
Thomas Collins is a freelance medical writer based in Florida.
Take-Home points
- Better methods are needed to identify the site of OSA.
- Radiofrequency tongue reduction can be an effective treatment, but not for patients with multiple severe contributing factors.
- TORS for tongue reduction can produce dramatic improvements in AHI, especially in patients with no prior surgery.
- Endoscopic coblation tongue base resection is an effective option for more severe cases.
- A neuromuscular component exists in OSA and epiglottis collapse.