More than 100 subtypes of HPV have been identified since the discovery that HPV causes cervical cancer, with specific types considered high risk as causative agents of cancer. Unlike cervical cancer, in which two types of HPV strains cause most anogenital cancers (HPV-16 and HPV-18), HPV-16 accounts for more than 90 percent of HPV-associated oropharyngeal cancers. It is thought that HPV disrupts the cell cycle and, for people who do not clear the infection, malignancy can occur when the tumor suppressor protein p53 and the retinoblastoma protein (pRb) are inactivated by the expression of viral E6 and E7 oncoproteins.
Explore This Issue
November 2012 “We think there is a long latency for progression of oral HPV infection into HPV-related head and neck cancers.”
“We think there is a long latency for progression of oral HPV infection into HPV-related head and neck cancers.”—Gypsyamber D’Souza, PhD
Although Dr. D’Souza said that the natural history of oral HPV is not well studied, she said the data suggest that it is similar to cervical cancer. For the minority of people who do not clear HPV infection on their own, the risk of developing disease increases the longer HPV persists.
“This is a very long process, and in the cervix it takes over 10 years from the time of infection to the development of malignancy,” she said. “We think there is likely a similar long latency for progression of oral HPV infection into HPV-related head and neck cancers.”
Unlike cervical cancer, however, there are no tests comparable to a Pap test to detect precancerous lesions in the oropharynx. “We don’t have a good screening option,” said Erich M. Sturgis, MD, MPH, professor in the department of head and neck surgery at The University of Texas MD Anderson Cancer Center in Houston. He added that the entire mucosal surface of the cervix is easier to examine than that of the tonsils and base of tongue, the two sites predominately affected by HPV-related oropharyngeal cancers.
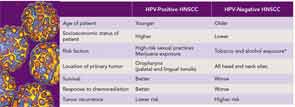
One ongoing challenge is to find a standard way to detect HPV-related oropharyngeal cancers to help tailor treatment for these patients (see “Tests Emerging as Standards for Diagnosing HPV-Positive Oropharyngeal Cancer,” p. 26). The importance of finding such a method is highlighted by studies that consistently show better survival in patients with HPV-related oropharyngeal cancers than those with non HPV-related cancers.
Survival Benefit in HPV-Related Oropharyngeal Cancers
A recent 2012 meta-analysis that pooled data from 42 studies found significant improvement in both progression-free survival and disease-free survival in patients with HPV-positive oropharyngeal cancers when compared with HPV-negative oropharyngeal cancers (Oral Oncol. [Published online ahead of print July 27, 2012.]). A similar benefit was seen in a retrospective analysis of patients with stage III or IV oropharyngeal squamous cell carcinoma enrolled in a randomized trial that compared survival outcomes of patients treated with accelerated-fractionation radiotherapy and those treated with standard-fractionation radiotherapy combined with cisplatin therapy. A total of 206 of 323 (63.8 percent) of patients had HPV-positive oropharyngeal cancers. After adjusting for age, race, tumor and nodal status, tobacco exposure and treatment assignment, the HPV-positive patients had significantly better three-year overall survival rates compared with the HPV-negative patients (82.4 percent versus 57.1 percent, p<0.001) (N Engl J Med. 2010;363(1):24-35).
Leave a Reply