INTRODUCTION
In recent years, the treatment of Zenker’s diverticulum (ZD) and other hypopharyngeal diverticula has undergone substantial transformation. Refinement in instrumentation and surgical technique have led to improvements in treatment outcomes and treatment-associated morbidity. Flexible endoscopic Zenker’s surgery has gained wider acceptance and has resulted in the ability to treat more patients with these disorders using minimally invasive endoscopic techniques previously relegated to only open approaches. Although gastroenterologists with training in advanced endoscopy have been performing tunneled peroral endoscopic myotomy over the past decade, few otolaryngologists and thoracic surgeons have been exposed to flexible endoscopic surgery in their training.
Flexible Zenker’s surgery is not a new phenomenon. The initial techniques described by Brazilian and Dutch groups in the mid-1990s used a flexible gastroscope with electrosurgical instruments fed through a working channel to simply divide the common wall or septum in a procedure called a standard septotomy. During the early days of the standard septotomy, a centimeter or more of the common wall was left undivided as a precaution against esophageal leaks; however, a 2013 series of 150 patients treated with standard septotomy reported short-term improvement in dysphagia symptoms but also found a 20% recurrence rate.
The Z-peroral endoscopic myotomy (Z-POEM) was developed to address the issue of recurrence while providing a safe post-operative result that minimized leaks. The submucosal tunneling (“third space” endoscopic surgery) and endoscopic myotomy techniques classically used at the lower esophageal sphincter for endoscopic achalasia treatment were adapted to the upper esophageal sphincter.
Our objective is to provide a path for otolaryngologists not familiar with advanced flexible endoscopic surgical techniques to build on their existing skills with rigid diverticulotomy to eventually gain the ability to perform a purely flexible Zenker’s surgery for patients who prefer an endoscopic approach but have anatomic factors that prohibit rigid exposure and comorbidities that preclude open surgery. Just as with rigid diverticulotomy surgery, the surgical goals are the same: to fully perform a cricopharyngeus muscle myotomy and divide the common wall so a food bolus will continue to flow distally during the swallow.
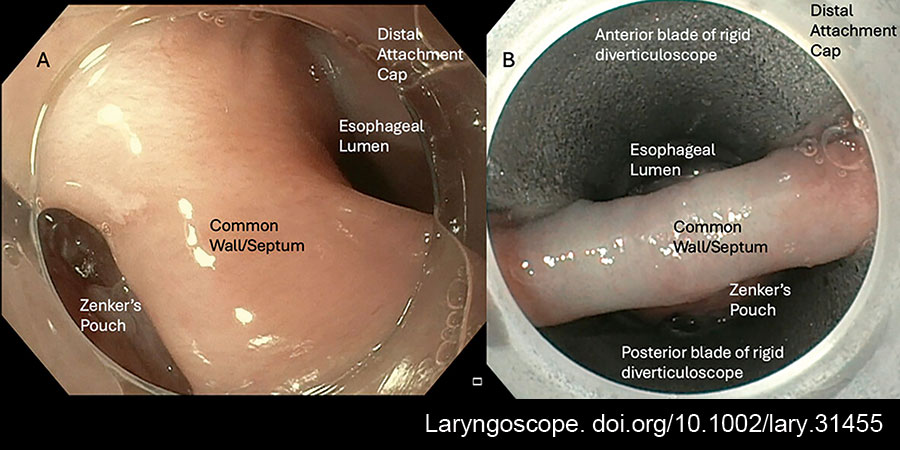
Figure 1: Image (A) shows the endoscopic view of the common wall through the Olympus H190 gastroscope with distal attachment cap; the diverticulum is to the left of the common wall and the esophageal lumen is to the right. Image (B) shows the common wall of the diverticulum exposed through a bivalved diverticuloscope with the esophageal lumen above and the diverticulum below the common wall. doi.org/10.1002/lary.31455
METHODS
The surgical technique in each of its components can be viewed in the online Supporting Video 1.
Z-POEM surgery is performed under general anesthesia with full neuromuscular blockade. We recommend this, as patient bucking and movement during POEM surgeries can increase the technical difficulty and lead to higher rates of pneumomediastinum, bleeding, and perforation. We prefer to keep the patient in a supine position but left lateral decubitus positioning is also possible, particularly in cases done using a purely flexible method.
Part I of the procedure is the diagnostic esophagoscopy and diverticulum exposure. An adult-sized gastroscope equipped with a disposable distal attachment cap is introduced transorally through a bite block. The distal attachment cap is key to assist with visualization and maximize working space, as maneuverability can be limited in the upper esophagus (Fig. 1). The diverticulum length is measured, and the pouch is cleared of debris. The esophagus and stomach are then inspected for any possible distal pathology that may also contribute to the patient’s dysphagia. Some endoscopists will place a guidewire or a nasogastric tube into the esophagus to aid with orientation during the procedure. This is not our practice, as after orientation is confirmed, it is relatively straightforward to maintain orientation with the diverticulum on screen left and the esophagus on screen right. CO2, used for insufflation, is quickly reabsorbed, resulting in less risk of post-operative pneumomediastinum. For surgeons first learning flexible advanced endoscopy, obtaining rigid exposure with a bivalved diverticuloscope and performing the Z-POEM technique through rigid exposure is a reasonable path to gaining experience with the new technique. Also, for diverticula filled with firm food debris, disimpaction can sometimes only be achieved with rigid instrumentation.
Part II involves positioning the gastroscope at the common wall of the diverticulum. Minimal submucosal blebbing is needed, and over injection can actually be disorienting to the surgeon. We recommend injecting a conservative amount of lifting agent, which allows for expansion of the submucosal space to allow for an isolated mucosotomy. We typically recommend 1% lidocaine with epinephrine 1:100,000. Using proprietary polysaccharide blends for lifting agents is typically not necessary for ZD surgery, and neither is using dyes like methylene blue or indigo carmine solution, as we find the distinction between mucosa and muscle fibers to be clearer without these dyes.
After the injection, a mucosotomy is made across the common wall using a monopolar electrosurgical instrument through the working channel of the gastroscope. A straight needle-type electrosurgical knife will cut through the mucosa, exposing the muscular aspect of the common wall (e.g., DualKnife J, Olympus Tokyo, Japan). The incision should be just wide enough to comfortably fit the diameter of the gastroscope with its distal attachment.
With regard to the monopolar cautery power source, we prefer to use the Erbe electrosurgical unit. For cutting through mucosa and muscle sharply without char, we use the Endo Cut Q setting with an effect of 2, cut duration of 1, and cut interval of 3. When bleeding or vascular tissue is encountered during the procedure, we use a forced coagulation mode with an effect of 2 and a maximal wattage of 50.
Part III focuses on dissecting the submucosa away from the muscular septum on both the esophageal and diverticulum sides. The monopolar knife is used to dissect the fibers away from each side of the muscular septum, taking care not to damage the mucosal layers. During dissection, we recommend erring on the side of cauterizing muscle, as this will be divided later in the procedure anyway. Many electrosurgical knives allow for additional submucosal injection through either the tip or base of the knife, which aids in easier and faster submucosal dissection.
Part IV is the myotomy, dividing the muscular aspect of the common wall. After submucosal tunneling and dissection are complete on both the diverticular and esophageal sides of the diverticulum, the muscle can be cut using various instruments. This is often completed with the same electrosurgical knife that is used for the mucosotomy and submucosal dissection, as this allows for precise myotomy down to the final remaining fibers. Other types of knives, such as scissor-type stag beetle (SB) knives, can also be used, as they quickly provide a clean and hemostatic cut. When using the SB knife, we use the Erbe Endo Cut Q settings with an effect of 1, cut duration of 1, and cut interval of 1, and when needing to divide small vessels and control bleeding, we use forced coagulation mode with an effect of 2 and a maximal wattage of 50.
The key to avoiding recurrence is making sure the myotomy is completed down to the base of the diverticulum. Z-POEM technique allows for excellent visualization of the entire muscular common wall. We recommend removing the gastroscope from the “third space” incision and moving it into the pouch and esophagus to check for inadvertent mucosal tears.
Part V, the final part of the POEM, is watertight closure of the incision. We recommend using short stem 11- or 16-mm endoscopic clips such as the ConMed Duraclip or the Micro-Tech Endoscopy Lockado. The clips are placed to bridge the edges of the mucosa, which apposes easily with the common wall muscle divided. We recommend clipping sequentially from top to bottom or vice versa, as the stems of the clips can interfere with positioning of subsequent clips, especially if placed in the middle of the incision initially. These endo-clips rarely lead to globus sensation and pass easily after the incision has healed. If an esophageal perforation is made during the procedure, this should be clipped, and a nasogastric tube should be placed until a post-procedure water-soluble contrast esophagram can confirm there is no leak.
In some cases, with a larger diverticulum, we advocate for a partial division of the mucosal septum, in addition to the classic muscular septotomy. This modification attempts to deal with the problem of the preservation of the mucosal aspect of the common wall, which is thought to lead to recurrence or persistence of symptoms. After a Z-POEM with partial mucosotomy, the appearance of the pharyngoesophageal segment will look somewhat similar to a patient who has had a CO2 laser diverticulotomy, which divides the septum down to its base.
RESULTS
Twenty-five patients on whom the described peroral endoscopic myotomy was performed from 2022 to 2023 were included. All the patients had pre-operative video fluoroscopic swallow studies or esophagrams confirming the diagnosis of Zenker’s diverticulum. Fifty percent of patients had stage I diverticulum measuring less than 2 cm in length, and 50% of patients were classified as stage II, measuring between 2 and 4 cm. Stage III diverticula (greater than 4 cm) are typically managed via an open approach by the senior author. All patients had pre-operative complaints of solid food dysphagia ± regurgitation, and the mean pre-operative EAT-10 decreased by 85.2% from 22.8 to 3.36 (p < 0.001). Objective fluoroscopic swallowing metrics (AP/Lateral UES opening and diverticulum size) also improved significantly. No patients reported serious complications or recurrence over a 12-month follow-up period. One patient did develop mild crepitus and neck discomfort after the procedure, which resolved with observation, IV antibiotics, and NPO status for two days, and the patient was able to resume the PO diet after the resolution of crepitus. This case did occur in our first five patients and likely resulted from an error with complete endo-clip closure.
CONCLUSION
These techniques have a steep learning curve but are appropriate for patients unable to undergo rigid diverticulotomy and in cases where open surgery is contraindicated or declined due to potential morbidity. These flexible techniques have been pioneered by our colleagues in gastroenterology, but surgeons have been performing Z-POEMs successfully, and otolaryngologists should continue to adopt a variety of techniques to provide our patients with a diverse array of surgical options tailored to the individual.