INTRODUCTION
Salvage nasopharyngectomy for recurrent nasopharyngeal carcinoma (NPC) is a morbid procedure. Sequelae may include velopharyngeal insufficiency (VPI), skull base osteomyelitis, and internal carotid artery (ICA) blowout syndrome, which carries a 60% risk of mortality. Robust reconstruction of the surgical defect is imperative, especially if re-irradiation of the field is to be considered. Nasoseptal flaps (NSFs) are the workhorses for the reconstruction of skull base defects; however, they present several drawbacks for the reconstruction of nasopharyngeal defects. The NSF is thin, and the tissue from which it is harvested may have withstood radiation for the primary treatment of NPC.
Explore This Issue
April 2025The ideal reconstruction would offer healthy vascularized tissue with adequate bulk to limit VPI and provide protection to the cervical ICA. The submental artery island flap (SMIF) offers a sizeable musculocutaneous flap with a reliable vascular pedicle, preventing the need for microvascular anastomosis. Additionally, the flap lies largely outside of typical radiation fields used for NPC, as the lymphatic drainage of the nasopharynx essentially bypasses the Level 1 nodal station.
The SMIF is commonly used for the reconstruction of skin and mucosal defects. Dissection of the vascular pedicle to the artery and vein of origin allows reliable reach for lateral skull base defects. Similarly, this long, narrow pedicle allows the flap to reach the nasopharynx and central skull base when directed along a more medial vector through the parapharyngeal space. This study details the utilization of a pedicled SMIF for reconstruction after endoscopic nasopharyngectomy in a patient with recurrent NPC.
METHODS
A 58-year-old male presented with recurrent (rycT2N0M0) NPC two years after the completion of definitive chemoradiotherapy (CRT) for his initial disease. MRI demonstrated recurrent tumor involving the right fossa of Rosenmüller, Eustachian tube, and parapharyngeal space with 180-degree contact of the parapharyngeal ICA (Fig. 1). There was no obvious perineural spread, intracranial extension, or extension to the prevertebral fascia. The patient underwent an expanded endoscopic endonasal approach (EEA) for salvage nasopharyngectomy. Reconstruction of the nasopharyngeal defect was accomplished with a pedicled SMIF to provide appropriate tissue bulk in the infratemporal fossa (ITF) and guard the ICA. Approval from the Institutional Review Board (IRB) was requested, and this project was determined to be
IRB-exempt.
RESULTS
A Denker’s extended medial maxillectomy was performed on the right, along with a complete ethmoidectomy and posterior septectomy to create a common sphenoid cavity. A left NSF was harvested and tucked into the ipsilateral maxillary sinus. The contents of the pterygopalatine fossa (PPF) were mobilized inferolaterally, and the greater sphenoid wing (GSW) and pterygoid plates were drilled to expose the ITF. The lateral pterygoid muscle (LPM) was elevated from the GSW and resected, exposing the foramen ovale and foramen spinosum. The parapharyngeal ICA was identified, and the tumor was dissected off the vessel. Tumor dissection continued medially along the prevertebral fascia. A right neck dissection was performed for vascular control and nodal sampling.
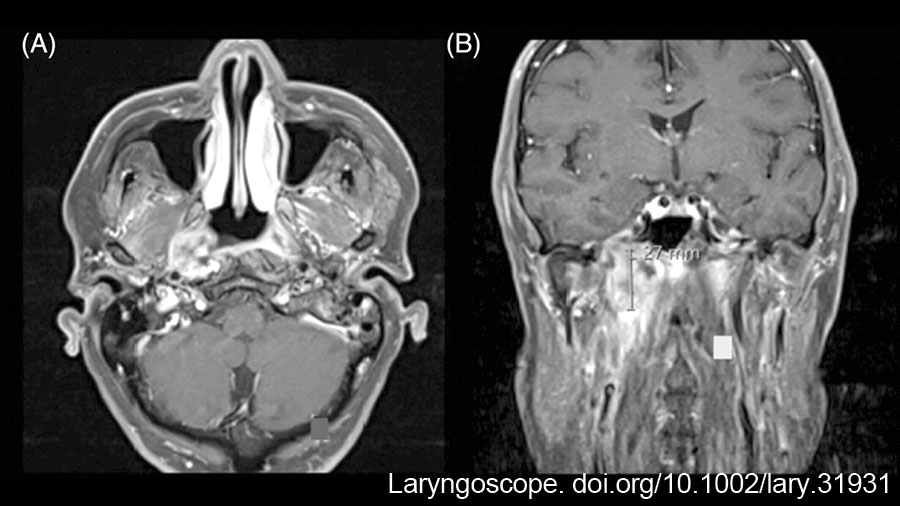
Figure 1: (A) T1-weighted MRI with gadolinium and fat saturation in the axial plane: Enhancing nasopharyngeal lesion centered in the right fossa of Rosenmüller, with extension to the prevertebral fascia, parapharyngeal ICA, and pterygoid plates; (B) Coronal plane: Enhancing right nasopharyngeal lesion, with extension superiorly into the mandibular strut of the greater sphenoid wing and foramen ovale, and laterally into the ITF and parapharyngeal space. ICA, Internal carotid artery; ITF, Infratemporal fossa. doi.10.1002/lary.31931
An SMIF was then harvested for reconstruction in the manner described by Patel and colleagues. (Laryngoscope. doi.org/10.1097/01.mlg.0000246519.77156.a4). The nasopharyngectomy defect was inspected and measured; a 4 × 6 cm skin paddle was designed in the submental skin. Subplatysmal flaps were previously raised in the neck dissection, and the marginal mandibular nerve was identified and mobilized superiorly. The submandibular gland was dissected from its fascial capsule and excised to allow identification of the facial and submental vessels (Fig. 2A). The anterior skin paddle incision was carried to the superficial layer of the deep cervical fascia. The integrity of the vascular pedicle was confirmed, and the skin paddle incision was completed. The flap was harvested from left to right (distal to proximal) by identifying and transecting the mylohyoid muscle in the midline and dividing the right anterior belly of the digastric muscle from the mandible and hyoid. The mylohyoid was then detached from the mandible and hyoid. The muscle was bluntly dissected from the middle layer of deep cervical fascia to mobilize the vascular pedicle (Fig. 2B). The facial artery and vein were ligated above the origin of the submental vessels, and the pedicle was dissected proximally to maximize its length (Fig. 2C). The parapharyngeal space had been exposed during tumor resection as the MPM was detached from its origin by drilling the pterygoid plates. Access to the parapharyngeal space in the neck was facilitated after dividing the mylohyoid muscle from the mandible during flap harvest. The tunnel for transposition of the SMIF to the nasopharynx was then created by simply releasing the stylomandibular ligament and dilating the parapharyngeal space through blunt dissection along the MPM (Fig. 2D).
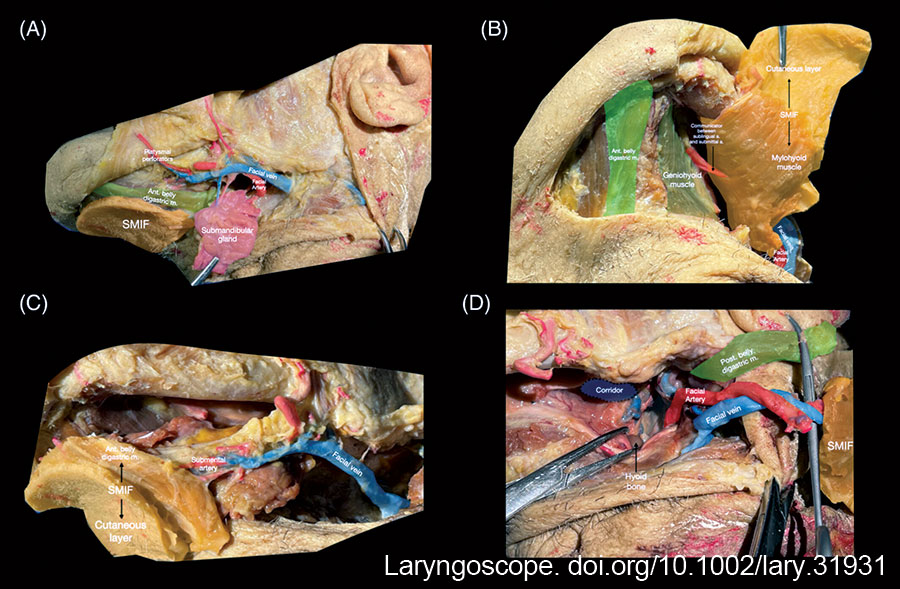
Figure 2: Harvesting the SMIF: (A) meticulous excision of the submandibular gland to preserve the submental vessels; the common facial and external jugular veins are preserved; (B) the mylohyoid muscle is divided at the midline raphe and released from the mandible and the hyoid; the ipsilateral anterior digastric is included to preserve perforating arteries. The flap is then bluntly dissected away from the geniohyoid muscle and middle layer of deep cervical fascia; the mylohyoid is included in the flap; (C) the myocutaneous SMIF may include a sizeable skin paddle along with submental fat and the anterior belly of the digastric muscle and mylohyoid muscle; (D) retrograde dissection of the facial artery to its origin from the external carotid artery maximizes pedicle length. A tunnel is dissected through the parapharyngeal space medial to the mandibular insertion of the medial pterygoid muscle to allow transposition of the flap into the nasopharynx. Ant, Anterior; M, Muscle; Post, Posterior; SMIF, Submental island flap. https://doi.org/10.1002/lary.31931
The skin paddle was de-epithelialized and passed to the nasopharyngectomy defect through the parapharyngeal corridor along the surface of a one-inch Penrose drain. To pass the flap, a traction suture was placed on the distal end of the skin paddle. Under endoscopic visualization, the flap was pushed cranially through the parapharyngeal space while pulling on the traction suture until it was seated in the surgical defect. Flap inspection revealed bleeding from its de-epithelialized surface, confirming the integrity of the vascular pedicle. Manipulation of the flap demonstrated that no further measures were necessary to secure it within the defect. Flap stabilization was provided by the tethering effect of the vascular pedicle within the narrow transposition corridor. The previously harvested NSF was rotated to cover exposed bone in the clival recess. Absorbable nasal packing was placed anterior to the flap in the maxillary sinus, maintaining patency of the nasopharynx. A temporary tracheostomy was performed to ensure a safe airway in the immediate post-operative period.
The final pathology was consistent with squamous cell carcinoma, and margins were reported negative. The patient underwent an endoscopic biopsy of the superior ITF four months after the procedure due to an area with concerning residual disease. This biopsy required partial mobilization of the SMIF, which was well integrated and possessed a robust blood supply. No residual disease was identified in the biopsy, and the patient had no evidence of disease 12 months after surgery.
CONCLUSION
Endoscopic nasopharyngectomy exemplifies both the technical progress in expanded endoscopic skull base surgery and its novel reconstructive challenges. The SMIF is well suited for reconstruction of nasopharyngectomy defects and may be useful more broadly for reconstruction of volumetric defects of the central skull base.
Leave a Reply