Introduction
A range of open and endoscopic approaches to the maxillary sinus have been described and used for the treatment of both rhinological and skull base disease. Endoscopic approaches to the maxillary sinus have largely replaced open techniques, but in selected scenarios open approaches are still necessary (J Laryngol Otol. 2020;134:473–480).
While a wide variety of pathologies of the maxillary sinus, pterygopalatine, and infratemporal fossa can be addressed through an ipsilateral or an open approach, contralateral approaches are useful for lesions seated laterally, anteriorly, and inferiorly in the coronal plane. Expanded approaches to these anatomical areas include the Caldwell-Luc, mega-antrostomy, medial maxillectomy, Denker’s, prelacrimal Denker’s, and transseptal. A transseptal approach enables improved access to challenging anatomical locations, particularly pathology seated in the anterior and lateral regions (Am J Rhinol Allergy. 2009;23:426–432). However, access maybe be limited by the height of the nasal floor and there is an increased risk of septal perforation (J Laryngol Otol. 2020;134:473–480). Septal perforation symptoms can vary depending on the size and the location of the defect; however, they include epistaxis, nasal obstruction, crusting, nasal discharge, cacosmia, and intermittent whistling, and have a negative impact on a patient’s quality of life. They can be difficult to manage and are a risk associated with any septoplasty. This article describes a transseptal approach by elevating bilateral mucoperichondrial flaps and approaching a lesion from the contralateral side, which offers an expanded window to the maxillary sinus. Additionally, we also demonstrate our technique for septal reconstruction after this approach.
Method
A 40-year-old African American male presented to an outside facility with a six-month history of nasal obstruction. In-office biopsy reported a nasal polyp, and he was scheduled to undergo middle meatal antrostomy, septoplasty, and inferior turbinate reduction. Intraoperatively, he was found to have an inverted papilloma. His surgery was then aborted, and he was referred to Augusta University Medical Center for further management. The patient was scheduled for a transseptal approach to the maxillary sinus and pterygopalatine fossa with septoplasty.
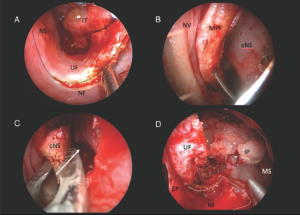
Figure 1. (A) Incision and elevation of “U”-shaped mucoperichondrial flap; the dotted line marks the area of incision. (B) Contralateral side mucoperichondrial flap sutured to the lateral nasal wall. (C) Removal of septal cartilage; the white arrow shows the transseptal window where the scope will pass. (D) Transseptal window showing exposure; the white dotted line marks the area where the “U”-shaped flap was raised. cNS = cartilaginous nasal septum; IP = inverted papilloma; IT = inferior turbinate; MPF = mucoperichondrial flap; MS = maxillary sinus; NF = nasal floor; NS = nasal septum; NV = nasal vestibule; UF = “U”-shaped flap.
We begin by raising a “U”-shaped mucoperichondrial flap of the ipsilateral nasal floor and part of the inferior meatus mucosa that is extended medially to the nasal septum (Figure 1, A). The incision is extended superiorly along the nasal septum so that the mucosal flap can be pushed posteriorly. Next, an inferior turbinate resection is performed. On the contralateral side, an incision is made along the choana and brought forward through the nasal floor. The mucoperichondrial flap is elevated conventionally. No superior incision is made, leaving the flap superiorly attached. This mucoperichondrial flap is sutured to the lateral nasal wall at the level of the alar vestibule to hold it in place (Figure 1, B). The septal cartilage is then removed and kept in saline for the septal reconstruction (Figure 1, C). After this, we pass the scope through the transseptal approach to widely expose the posterior wall of the maxillary sinus (Figure 1, D). With this wide approach and enhanced visualization, we perform four-handed dissection and bilateral instrumentation to achieve en bloc resection of the tumor with straight instrumentation. After resection of the tumor, the “U”-shaped flap is repositioned along the nasal floor covering part of the medial maxillectomy defect. The septal cartilage is wrapped in Gelfoam and repositioned to aid in mucosal healing and prevent a postoperative septal perforation. The mucoperichondrial flap is repositioned and closed conventionally with 4–0 chromic sutures, and Doyle splints are placed to prevent adhesion formation and are removed two weeks postoperatively.
Results
Through this approach, the inverted papilloma was resected en bloc and the patient’s recovery was uneventful. Three months postoperative nasal endoscopy showed a well-healed septum with no residual septal deviation or septal perforation.
This transseptal technique allows a wide window exposure with enhanced visualization of the maxillary sinus, which enables a straight four-handed dissection and bilateral instrumentation, as well as clear visualization. Our instruments can reach more laterally compared to a unilateral approach, as evidenced by closeness to the proximal aspect of the infraorbital nerve within the maxillary sinus exhibited on intraoperative imaging. We demonstrate our septal repair, and postop nasal endoscopy five months after surgery reveals a well-healed straight nasal septum without septal perforation. The supporting video illustrates the key points of the operative technique used to remove the lesion and reconstruct the nasal septum.