Introduction
The goal of cholesteatoma surgery is to completely remove the disease, to restore hearing when possible, and to prevent residuals and recurrence. The prevention of recurrence is dependent on the quality of the tympanic membrane (TM) reinforcement and the reconstruction of the external auditory canal (EAC) in order to oppose a new TM retraction pocket. The prevention of residuals requires complete removal of the cholesteatoma, relying on optimal visualization of the anatomical spaces harboring the disease. The epitympanum is a prime area for the development of cholesteatoma. Access can be limited with a transcanal microscopic approach, requiring an antromastoidectomy. The transcanal endoscopic approach offers a magnified view of this space and 0° to 45° angled endoscopes. Extensive removal of the scutum posteriorly opens a wide access to the posterior epitympanum and aditus ad antrum. Cartilaginous reconstruction of the scutum should allow excellent stability of the cartilaginous grafts and seal with the tympanal bone to prevent further pars flaccida retraction.
This extensive reconstruction procedure, however, remains difficult in a one-handed endoscopic technique. Obliteration of the mastoid, sometimes associated with the epitympanum in microscopic cholesteatoma surgery, is thought to bring about a reduction in the rate of recidivism (residuals and recurrences). Their application to endoscopic surgery has so far never been reported. This case presents a transcanal endoscopic procedure for cholesteatoma with epitympanic obliteration using bioglass.
Method
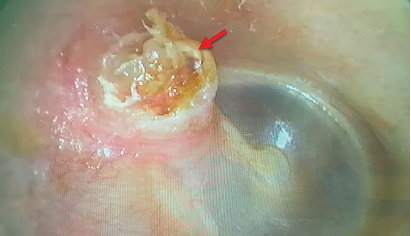
Figure 1a. Preoperative otoscopic examination (red arrow: pars flaccida cholesteatoma).
A transcanal endoscopic approach was performed with the aim of removing an epitympanic cholesteatoma (Figure 1a) without the transmastoid approach, and to reconstruct the scutum after obliteration of the epitympanum at the same time. The preoperative temporal bone CT scan revealed an anterior and posterior epitympanic cholesteatoma without extension into the antrum, a sclerotic mastoid, an overhang of the sigmoid sinus, and a bone erosion of the anterior tegmen tympani. Rigid 0° and 45° angled, 14-mm long, 3-mm diameter endoscopes were used and coupled with a high-definition 3CCD camera and video system. Bone removal from the scutum was adapted to the extension of the cholesteatoma and performed by an underwater endoscopic drilling. Total obliteration of the epitympanum was achieved using 45S5 bioactive glass. Perichondrium was placed to seal off the aditus ad antrum and to prevent possible migration of the Glassbone inside the
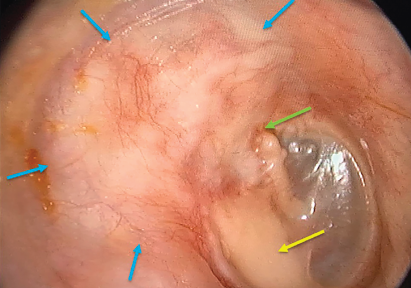
Figure 1b. Postoperative otoscopic examination after 1 year (blue arrows: margins of the epitympanic obliteration; green arrow: contact with the malleus; yellow arrow: ossiculoplasty using cartilage).
© Ayache S. Laryngoscope. doi:10.1002/lary.29710
mastoid, which could secondarily lead to a reduction in the volume of the epitympanic obliteration and a retraction of the cartilages. Moreover, this material must be carefully packed to avoid any cavities within the obliteration. The Glassbone was positioned from the anterior epitympanum to the aditus ad antrum, without bulging in the EAC to prevent any postoperative stenosis.
Reconstruction of the scutum was performed using cartilaginous and perichondrium grafts harvested from the tragus and covering the entire surface of the obliteration. The grafts were placed paying particular attention to the sealing between them to avoid any leakage of the Glassbone in the ear canal and to prevent any secondary retraction of the grafts. An ossiculoplasty was performed using a cartilaginous piece between the stapes and the TM. No intraoperative intravenous antibiotic therapy was given. The patient was sent home the day of surgery with a prescription of local antibiotics for 10 days. The study has been performed according to the Declaration of Helsinki (see supporting video).
The texture of the 45S5 Bioactive Glass was well suited for the epitympanic obliteration using a one-handed endo-scopic technique.
Results
No pre- or postoperative complications occurred. The texture of the 45S5 bioactive glass was well suited for the epitympanic obliteration using a one-handed endoscopic technique. The healing of the EAC was complete without leakage of the Glassbone. After one postoperative year, the patient had a self-cleaning intact ear canal, without stenosis (Figure 1b). The first diffusion-weighted imaging magnetic resonance imaging performed at one postoperative year was negative.