INTRODUCTION
Treatment of primary epiglottis collapse (EC) in patients with obstructive sleep apnea/hypopnea syndrome (OSAHS) still presents a challenge. Drug-induced sleep endoscopy (DISE) (Laryngoscope. 2015;126:515–523) has allowed assessment of the prevalence of EC in 10% to 40% of patients suffering from OSHAS. In order to treat this condition, we developed a minimally invasive technique called an epiglottis stiffening operation (ESO) (Acta Otorhinolaryngol Ital. 2019;39:404–408). ESO has been shown to be a safe and easy-to-perform procedure, with great efficacy and very short surgical training required. Herein, we propose standardization of this technique by describing the surgical procedure in detail, including some tips and tricks.
Explore This Issue
October 2022METHOD
All patients who underwent ESO between Jan. 1, 2015, and Dec. 31, 2020, at the Department of Otorhinolaryngology of Humanitas San Pio X were enrolled for the study. During the preoperative diagnostic work-up, each patient underwent a complete physical and endoscopic evaluation, polysomnographic study (PSG), and DISE. DISE was always performed by an expert otolaryngologist and recorded and later collegially discussed among the otolaryngologist surgeon, neurologist, pneumologist, and odontologist. All treatment options, including custom surgery, were proposed to the patients. Epidemiological and clinical data, surgical reports, outcomes, complications, and follow-up information were reviewed.
Surgical Technique. Exposition of the epiglottis in direct microlaryngoscopy is performed using a traditional laryngoscope after mouth guard application. In this phase, the lingual side of the epiglottis totally (or almost totally) occupies the field of the laryngoscope, and its free edge touches the lower edge of the laryngoscope itself. The working area is identified as a rectangular area extended 1/3 in the upper half and 2/3 in the lower half of the epiglottis, between the lateral glossoepiglottic folds (including the median glossoepiglottic fold). Using a Kleinsasser suction cautery (outer diameter 3 mm and working length 26 cm) with an Erbe system set in the forced coagulation mode (50 watt max.), the exuberant mucosa included in the working area is raised and so cauterized, causing an immediate and visible retraction of the epiglottis.
In this phase, it is important to reach the perichondrium in order to induce stiffening and scar retraction of the tissues as a result of healing. The cauterization stops when the epiglottis free edge is seen more or less in the middle of the surgical field. During this step, it is mandatory to preserve the free margin of the epiglottis. The procedure ends by removing the excess cauterized tissue using a Cottonoid soaked in physiological water. The laryngoscope is retracted and the mouth guard is removed.
Contraindications. Body mass index (BMI) > 35 and anatomical features (e.g., trismus, mandibular prognathism) making laryngeal exposure difficult represent contraindications for this technique. Furthermore, this procedure is not indicated when a bulky tongue base pushes the epiglottis backward (secondary EC).
Postoperative Management. The Verbal Numerical Rating Scale 11 (vNRS-11) and Eating Assessment Tool 10 Italian version (I-EAT- 10) questionnaire were administered postoperatively. Patients were discharged on the first postoperative day with oral antibiotics therapy consisting of a third generation Cephalosporins (e.g., cefixime) once daily for seven days and a smooth and cold diet for seven to 10 days. Corticosteroid administration is not necessary. Patients were followed for at least six months postoperatively; endoscopic evaluation on the seventh and 30th postoperative days and PSG at three months were always performed.
RESULTS
From January 2016 to December 2020 we performed 536 surgical OSAS procedures, identifying a total of 109 patients with primary EC. Twenty-two patients underwent ESO within a multilevel snore surgery and were therefore ruled out, while 87 patients who underwent ESO exclusively fulfilled the inclusion criteria.
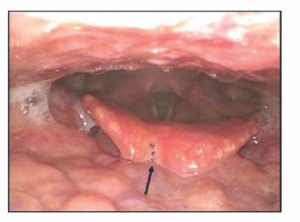
Figure 1. Postoperative onset of a notch of loss of substance caused by a vigorous manipulation of the epiglottis during the procedure. Example of improper healing of the epiglottis after an epiglottis stiffening operation
A strong prevalence of males was found; only 10 patients were women (11.5%), while 77 were men (88.5%); the mean age was 53.1 years old. The mean BMI was 26.8 kg/m2. Fourteen (16.1%) patients were affected by simple snoring and 73 (83.9%) patients were affected by OSAHS with a mean apnea/hypopnea index (AHI) of 30. The postoperative course of all patients was regular and substantially without pain, with discharge on the first postoperative day. Moreover, no patient had dysphagia, aspiration, or dysphonia. Two patients affected by diabetes mellitus had postoperative epiglottitis treated with oral antibiotics and resolved within six days. Postoperative fiberoptic endoscopic evaluation on the seventh and 30th postoperative days showed a consistent retraction of the epiglottis in all the patients. In three cases, loss of substance on the free edge of the epiglottis was found during the second postoperative examination (Figure 1). The mean postoperative AHI was 7.3, the mean postoperative snoring time was 11.2, and the mean Epworth Sleepiness Scale score was 6.3. Follow-up lasted from six to 68 months (see the supporting video.)