INTRODUCTION
Nasoseptal perforations (NSPs) have a variable etiology. The most common causes are iatrogenic (nasal surgeries), trauma, nose picking, nasal substance abuse, systemic inflammatory diseases, or chemical exposures. Reduction of crusting can be achieved with intranasal humidification, irrigation with isotonic saline, local application of antibiotic ointments, and topical emollients. Unfortunately, septal buttons have been associated with many complications such as pain, epistaxis, irritation, and crusting, and may contribute to a steady erosion of the perforation edges and eventual enlargement of the defect.
Explore This Issue
July 2023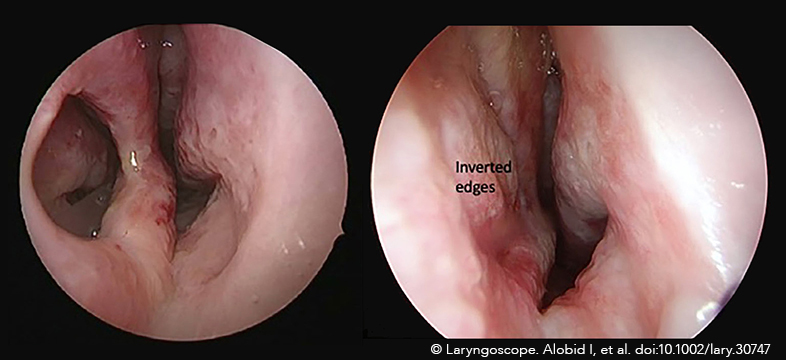
There is currently abundant literature advocating various methods of NSP repair. A recent survey by members of the American Academy of Facial Plastic and Reconstructive Surgery and the American Rhinologic Society demonstrated that the respondents had a similar preference for the endoscopic and external rhinoplasty approaches, followed by the endonasal approach. This study concluded that surgeons favored NSP repair using bilateral intranasal mucosal advancement flaps with an interposition graft (Facial Plast Surg. 2019;35:78–84).
Many endoscopic techniques for NSP repair have been developed. Anterior ethmoidal artery flap is the most commonly used endoscopic technique with a high success rate (Arch Facial Plast Surg. 2011;13:411–414; Laryngoscope. 2022;132:298–300). Recently, Mariño-Sanchez et al (Fac Plast Surg Aesthet Med. 2020;22:301–303) described a purely endoscopic surgical repair of NSP with a unilateral rotation septal flap pedicled to the greater palatine artery (GPA). The authors demonstrated that closure of very anterior NSP through an endoscopic endonasal approach can be achieved with a unilateral rotation mucosal flap based on the GPA. Additionally, in a radiological study and case series, Santamaría-Gadea et al (Eur Arch Otorhinolaryngol. 2021;278:2115–2121) demonstrated the feasibility of using this flap to close large NSPs. This procedure depends upon intact septal cartilage surrounding the perforation and is therefore not applicable in those cases in which a prior septoplasty has removed such cartilage.
Based on the original description of the GPA flap, and even though identifying the pedicle by direct vision may corroborate flap vascularization (Eur Arch Otorhinolaryngol. 2021;278:2115–2121), dissecting around the pedicle in a narrow space to achieve proper rotation of the flap may be difficult and risky because the artery could be accidentally damaged. Furthermore, following incisions described by the authors could generate a bulky pedicle and make the reconstruction more difficult, potentially producing nasal obstruction at the inferior level of the nasal valve. The Racket-on-Donut technique, as a modification of GPA flap, aims to simplify the procedure and improve postoperative outcomes.
METHOD
This is the description of the Racket-on-Donut technique, step by step:
- The incisive foramen is located using a ruler and marked at 1.5 cm from the anterior nasal spine or at the point previously measured in the CT scan, if available.
- Septal osteo-cartilaginous support is palpated, and the nasal mucosa is infiltrated either with a solution of bupivacaine (0.25%) and epinephrine (1:100,000) or saline. The infiltration must be performed in a subperiosteal and subperichondrial plane.
- The racket-shape flap should be one third bigger than the NSP. Once the flap size is estimated, the posterior incision starts 1 cm below the olfactory neuro-epithelium and extends downwards until it reaches the nasal floor, 2 cm posterior to the previously marked incisive foramen.
- An anterior incision is made as high as needed and extended downward through the posterior border of the NSP to the nasal floor, 1 cm anterior to the incisive foramen. Both anterior and posterior incisions are joined superiorly with an incision parallel to the skull base.
- A circumferential donut-shaped incision around the perforation in its superior, anterior, and inferior aspects is performed. NSP margins must not be refreshed to avoid damaging the inverted edges (IE) flap. A small anteriorly based triangle in the anterior portion of the donut-shaped flap is excised.
- The modified GPA (mGPA) mucoperichondrial/mucoperiosteal flap is harvested starting at the superior incision and advancing downward to the nasal floor. The mucoperichondrium around the perforation (IE) is elevated toward the perforation edges and flipped to the contralateral nasal cavity.
- The mGPA flap is rotated anteriorly and then sutured to the remnant mucosa with an absorbable suture. Silicone nasal splints are fixed to the columella and left in place for four weeks. No nasal packing is needed.
RESULTS
A series of 13 patients (39.2 years from 18 to 65 years; 6 female) with anterior NSP is presented. The etiology was nose picking (n = 6), drug abuse (n = 6), and previous nasal surgery (n = 1). All NSPs were located in a position anterior to the incisive foramen. The antero-posterior and supero-inferior NSPs diameters were 16.7 (10–27 mm) and 14.8 (10–25 mm), respectively. All cases were repaired by mGPA and IE without interposition grafts. Two months after surgery, both mGPA and IE flaps were completely integrated to the septal mucosa, and the osteo-cartilaginous septal support that had been left denuded during surgery showed complete reepithelialization (Figure 1, above; supplemental video). The main follow-up was 16.4 (6–38 months). No complications were observed.
