INTRODUCTION
As a surgical procedure to implant an electronic medical device, cochlear implantation is subject to not only complications related to open procedures, but also those related to device failure, implant migration, and off-target stimulation, among others. Device migration remains one of the more common complications of cochlear implantation, and a variety of surgical techniques have been developed to fix cochlear implants (CIs) in place (Otol Neurotol. 2021. doi:10.1097/MAO.0000000000003108). Improvements in device design and surgical techniques have resulted in a reduction in surgical cochlear implant revision rates (2.9% from 6%) over the past two decades (Otol Neurotol. 2021. doi:10.1097/MAO.0000000000003108; Laryngoscope. 2020. doi:10.1002/lary.28071).
Broadly, fixation methods can be divided into the bony-bed technique, in which a bone well is drilled into the calvarium to accommodate device placement, and the tight periosteal pocket technique, which fixes the device under blunt-elevated pericranium. Either technique can be modified with suture tie-downs, historically either in drilled channels in the cranial cortex, or directly to the periosteum (Otol Neurotol. 2021. doi:10.1097/MAO.0000000000003108). A systematic review comparison of these techniques did not demonstrate a significant difference in implant migration rates between the two general categories, but tie-down techniques were not included in the comparison (Otol Neurotol. 2021. doi:10.1097/MAO.0000000000003108). Single-center studies of a bony well technique with bone-channel suture tie-down report very low revision rates (two devices in 1,065 devices total) (Otol Neurotol. 2017. 2021. doi:10.1097/MAO.0000000000001302) and significantly lower migrations compared with periosteal pocket techniques (J Laryngol Otol. 2018. doi:10.1017/S0022215118000609).
In this study, we describe a time-saving modification of a bony-bed technique that utilizes screw-fixated Mersilene cervical cerclage suture, originally designed for treatment of uterine cervical insufficiency, as a simple, quick, and effective method for tie-down receiver/stimulator fixation. In our series, this modification of a tie-down technique resulted in no revision surgeries for receiver/stimulator migration, without longer operative times.
METHOD
Surgical Technique
Cochlear implantation technique was performed by a standard postauricular mastoid approach. A #4 cutting burr was used to drill a seat for placement of the implant. A trough was then drilled from the seat to the mastoid. The anterior edge of this seat was approximately 8–10 mm from the posterior edge of the mastoid.
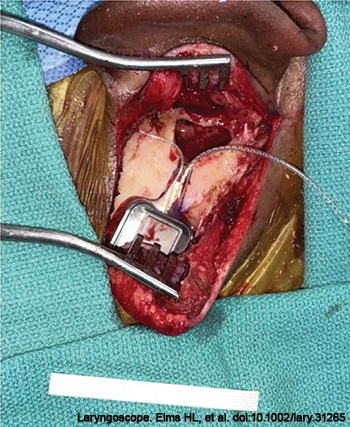
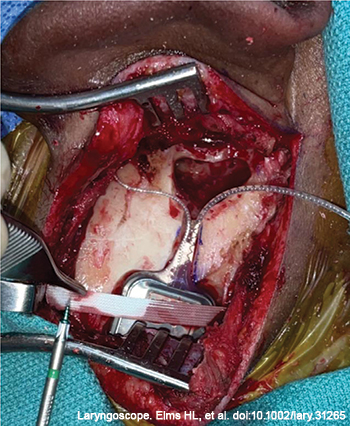
Figure 1. The cochlear implant is placed in the seat and trough; cervical cerclage tape is displayed on the drape.
The implant was opened and positioned in the drilled seat, with electrodes oriented anteriorly toward the planned cochleotomy (Figure 1). One-quarter-inch cervical cerclage tape was draped superoinferiorly across the implant receiver/stimulator and tightly secured to the bone with two 4-mm self-tapping titanium screws (Figure 2). With the implant receiver/stimulator secured, either a cochleostomy or atraumatic round window insertion was performed. This technique can be used to secure the receiver/stimulator of any of the available cochlear device brands.
To evaluate the efficacy of this technique, a retrospective patient data analysis was conducted using deidentified patient data according to a Duke University Institutional Review Board-approved exemption (protocol no. 00108742). Our institutional surgical database was queried by Current Procedural Terminology code for CIs performed between July 2013 and July 2022 at a single site. Patient operative reports were manually reviewed, and all patients whose reports described the above technique were included in analysis. Average operative times for these cases were extracted. Routine follow-up for patients included a two-week postoperative with the surgeon, one-month activation appointment with an audiologist, and annual audiologic appointments. Clinic notes and operative reports were reviewed for documentation of wound infections and revision surgeries for receiver/stimulator migration. Analyzed patient demographics included age, sex, and bilaterality of implants. Numerical and statistical analysis was performed using statistical functions within Microsoft Excel.
RESULTS
Between July 2013 and July 2022, 146 adolescent and adult patients underwent CI with the cerclage tape “seatbelt” technique. A total of 166 patient ears (20 bilateral implantations) were implanted during this interval. Seventy-nine (54.1%) patients were male. Age at first implantation ranged from 14 to 91 years (median 66.5).
Among implanted ears, there were zero instances of receiver/stimulator migration requiring surgical revision. Average operative time with the “seatbelt” technique was 107 minutes. There were no reported surgical site infections, device extrusions, or adverse reactions to the cerclage tape during the study interval. All but one patient (145 of 146, or 99.3%) presented for their activation appointments, and 84.9% were present at one-year audiologic follow-up. Follow-up intervals for this cohort ranged from one to 110 months (median 24).