Introduction
Jugular foramen paragangliomas (JFPs) are highly vascularized tumors. Although JFPs grow slowly and are considered histologically benign, the infiltrative nature of these tumors tends to destroy vital neurovascularities adjacent to the tumor. Since the infratemporal fossa type A approach (IFTA-A) was developed by Ugo Fisch, MD, the IFTA-A with total anterior transposition of the facial nerve (FN) and high cervical exposure has been the standard surgical procedure for removing JFPs (J Laryngol Otol. 1978;92:949-967). Traditionally, during anterior FN translocation, the FN was dissected from the geniculate ganglion to the main trunk of FN in the parotid gland to achieve permanent translocation; this procedure sacrificed the blood supply of the FN from the stylomastoid and deep petrous arteries, with a postoperative FN function (H-B I–II) of 67.2% (J Laryngol Otol. 2016;130:219-224). To preserve more feeding arteries of the FN, Dr. Brackmann (Otolaryngol Head Neck Surg. 1987;97:15-17) dissected the FN, the posterior digastric muscle, and soft tissues around the stylomastoid foramen anteriorly. Postoperatively, preserved FN function (H-B I–II) was noted in 73% of patients. However, it is still challenging to consistently achieve tension-free total FN anterior rerouting while applying Dr. Brackmann’s technique.
In the present study, we modified Dr. Brackmann’s total anterior FN rerouting technique to achieve tension-free FN anterior transposition and explored the surgical outcomes postoperatively.
Method
We conducted a retrospective review of the clinical data of patients with JFPs who underwent surgical management via the IFTA-A with tension-free FN anterior transposition at the otology and skull base surgery department of Fudan University in Shanghai, China, between April 2013 and September 2019. Only patients with JFPs who had normal FN function preoperatively according to the House-Brackmann (HB) grading system were included. This study was approved by the institutional review board of Fudan University.
We modified Dr. Brackmann’s total anterior FN rerouting technique to achieve tension-free FN anterior transposition and explored the surgical outcomes postoperatively.
All patients underwent temporal bone high-resolution computed tomography and magnetic resonance imaging (MRI) with gadolinium enhancement, magnetic resonance arteriography, and magnetic resonance venography. Digital subtraction angiography with super-selective endovascular embolization was performed 48 hours prior to surgery. Tumors were classified based on the Fisch classification system. The first follow-up of temporal bone MRI with enhancement was conducted three months postoperatively. Subsequently, the patients were evaluated every 12 months. Gross total resection (GTR) was defined as complete tumor excision without residue on temporal bone MRI. Tumor recurrence was defined as the occurrence of a new contrast-enhanced lesion in situ following GTR.
Surgical Procedures. The standard IFTA-A was applied in all patients, and several modifications were made to reduce FN tension during total anterior transposition (Figure 1; supporting video):
- The FN was dissected from the genicular ganglion to the stylomastoid foramen, the digastric muscle was detached from the digastric ridge, and the FN was dissected from the stylomastoid foramen and further dissected to the surface of the styloid process. Then the FN, the digastric muscle, and the parotid gland were anteriorly displaced (the main trunk of the FN in the parotid gland was not dissected). The parotid gland was sutured tightly to the lower margin of the temporal muscle to shorten the distance from the geniculate ganglion to the main trunk of the FN in the parotid gland.
- A long articulated retractor was placed at an angle of 45° to push the posterior belly of the digastric muscle and the parotid gland anteriorly and superiorly to further minimize the distance from the genicular ganglion to the main trunk of the FN in the parotid gland.
Statistical Analysis. Continuous variables are presented as medians and ranges, and categorical variables are presented as frequencies and percentages.
Results
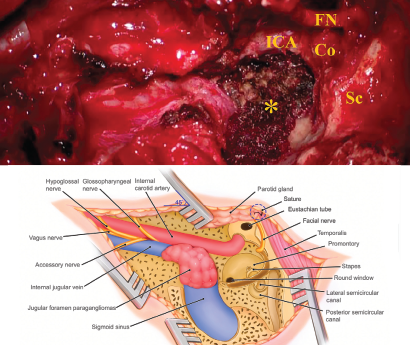
Figure 1. Schematic illustration of the infratemporal fossa type A approach (IFTA-A) with tension-free anterior rerouting of the FN. A) This intraoperative photograph shows the surgical field around jugular foramen after removing the jugular foramen paragangliomas with the modified surgical procedures. B) This illustration demonstrates anatomic structures around the jugular foramen following tension-free anterior rerouting of the facial nerve. Co = cochlea; FN = facial nerve; ICA = internal carotid artery; Sc = semicircular canal: * = jugular bulb, while the tumor was removed, and inferior petrous sinus was packed with Surgicel.
© Kong D, et al. Laryngoscope. DOI: 10.1002/lary.29658
The study included 15 women and five men, with a mean age of 49.58 years (range: 24–69 years). Eight (40%) and 12 (60%) patients were diagnosed with Fisch class C2 and C3 tumors, respectively.
GTR was achieved in 19 patients (95%). One patient did not obtain GTR due to extensive intraoperative bleeding and tumor infiltration of the internal carotid artery. Eighteen patients (90%) had an estimated blood loss of 100 to 450 mL (mean: 265 mL). The blood loss in the other two patients was 1,000 mL and 1,200 mL. Overall, the average blood loss was 360 mL, and the mean surgical time was 3.97 hours (range: 2.92–4.75 hours).
The preoperative FN function was HB grade I in all patients. FN function was HB grade I–II in 18 patients (90%) at the last postoperative follow-up. These patients had a positive response to an electrical stimulation of 0.5 mA after tumor removal, while an FN monitor was applied intraoperatively. The remaining two patients showed HB grade III FN function.
Five patients (25%) displayed dysfunction of the preoperative lower cranial nerves (CNs). One patient (5%) experienced newly developed lower CN IX deficit postoperatively. Cerebrospinal fluid leakage occurred in one patient (5%) intraoperatively; this leakage was successfully repaired with a muscle plug and abdominal fat packing. One patient (5%) experienced brain infarction on postoperative day three; this patient recovered completely. There was no other complication associated with surgery. One patient with GTR was recurrent four years postoperatively. The duration of follow-up ranged from 15 to 94 months (mean: 43.35 months).