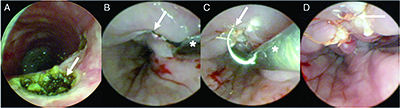
Figure 2. (A) Bronchoscopy demonstrating cauterization of tracheoesophageal fistula (TEF) (arrow). (B) Esophagoscopy in suspension showing rigid suction catheter (*) used to deliver Bugbee cautery to TEF site (arrow). (C) Microlaryngeal needle driver (*) holding suture needle (arrow). (D) Sutured TEF from esophageal lumen (arrow).
The patient was intubated with a 4.5-mm cuffed endotracheal tube (ETT) over a 4-mm telescope with cuff placed distal to the TEF. The esophagus was suspended with an adult Weerda distending operating laryngoscope (Fig. 1). A size 4 bronchoscope (Karl Storz, Germany) was inserted down the esophagus and through the TEF to ensure the ETT cuff was distal to the TEF. The FiO2 was decreased to 30%, and a Bugbee electrode cautery was placed down the side port of the bronchoscope to denude the edges of the TEF circumferentially on a setting of 15 W. Three 5-0 Vicryl sutures, 70-cm length on a TF needle (#J433), were placed using a Kleinsasser needle holder, microlaryngeal instruments, and a knot pusher (Karl Storz, Germany) to approximate the edges of the TEF. The procedure lasted approximately 1.5 hours. The patient was intubated with an endoscopically placed 5.5-mm cuffed ETT past the repair for the wakeup, sent to recovery extubated, and fed through his gastrojejunostomy tube.
Explore This Issue
July 2024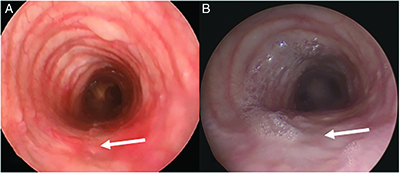
Figure 3. (A) Bronchoscopy demonstrating healed repair site after three months (arrow), and (B) after six months (arrow).
Despite the patient being asymptomatic, a persistent TEF was noted on the postoperative barium esophagram 18 days later. The decision was made to attempt closure for a second time by denuding the edges of the TEF more thoroughly and additionally on the tracheal side, and by placing more sutures than had previously been used. Rigid bronchoscopy was performed using a size 5 bronchoscope with 2.9 mm telescope. The tracheal surface of the TEF was cauterized using a Bugbee cautery down the side port on a setting of 30 W (Fig. 2). He was intubated over a telescope using a 5.0 cuffed ETT with the cuff placed distal to the TEF. The esophagus was suspended with an adult Weerda distending laryngoscope (Fig. 1). The FiO2 was decreased to 30%, and a Bugbee cautery was placed inside a rigid suction catheter that was bent to have a slight curve (Fig. 2). Delivering the Bugbee through the suction allows easier guidance, either through the tip for straight guidance or the velvet eye for curved guidance, and the ability to suction smoke for better visibility. This was placed down the esophagus under microscopic visualization, and the cautery was used on a setting of 30 W to denude the edges of the TEF circumferentially. Four 5-0 Vicryl sutures (#J433, 70 cm, TF needle) were placed from left to right with needle driver loaded backhand using microlaryngeal instruments and a knot pusher (Fig. 2). Repeat bronchoscopy was performed to ensure the ETT cuff had not inadvertently been sutured to the repair. The procedure lasted approximately two hours. The patient was extubated and sent to recovery in stable condition. Post-operative barium esophagram confirmed the TEF was closed six weeks later, and rigid bronchoscopy three and six months later during intubation for scoliosis repair confirmed a well-healed full-thickness repair (Fig. 3). Institutional research ethics board approval was waived for this case report.
CONCLUSIONS
Suspension microesophagoscopy in children can allow good visualization of the esophagus and a two-handed approach (four-handed if two surgeons) to facilitate closure of difficult-to-treat TEFs. TEF closure via the esophagus allows (1) access where suturing may not be possible in the smaller tracheal side, (2) intubation to prevent desaturation, (3) more time for the surgeon to accurately place sutures, (4) placement of knots in the esophageal lumen to decrease granulation tissue formation in the trachea. Further use of this exposure is required in younger children to determine if this technique is a viable alternative for endoscopic closure of difficult-to-treat H type TEF.