INTRODUCTION
Invasive thyroid carcinoma has well-documented routes of invasion to the upper aerodigestive tract (Laryngoscope. 2019;129:E455–E459). The most commonly invaded structures within the upper aerodigestive tract are the recurrent laryngeal nerve (RLN) (33%–51%), the strap and sternocleidomastoid (SCM) muscles (43%–78%), the trachea (4%–46%), the esophagus (9%–31%), and the larynx (12%–24%) (Head Neck. 2020;42:2741–2744; Otolaryngol Clin North Am. 2010;43:301–328).
Explore This Issue
June 2023Typically, tracheal invasion is treated surgically with circumferential tracheal resection or the previously published stair-step technique (Laryngoscope. 2019;129:E455–E459). However, when either is performed, there is risk of anastomotic complications, including the formation of intraluminal granulation tissue, anastomotic separation, stenosis, and fistulization. Anastomotic breakdown varies depending on the number of tracheal rings resected and other variables that may impair wound healing. In the short term, the risk of tracheal disruption with leakage of air and secretions poses the most significant risk to the patient. Depending on the magnitude of that anastomotic disruption, it, in turn, may lead to tracheal stenosis due to scarring. Although the SCM flap has been reported for use in augmenting tracheal repair, the authors present a novel tracheal reconstructive technique designed to incorporate the SCM muscle flap directly over the tracheal suture line to minimize the risk of anastomotic complications. It is presumed that the value of the SCM flap to participate in the wound healing process and to prevent air escape is dependent upon direct adherence of the muscle to the suture line and avoidance of dead space over that repair.
METHOD
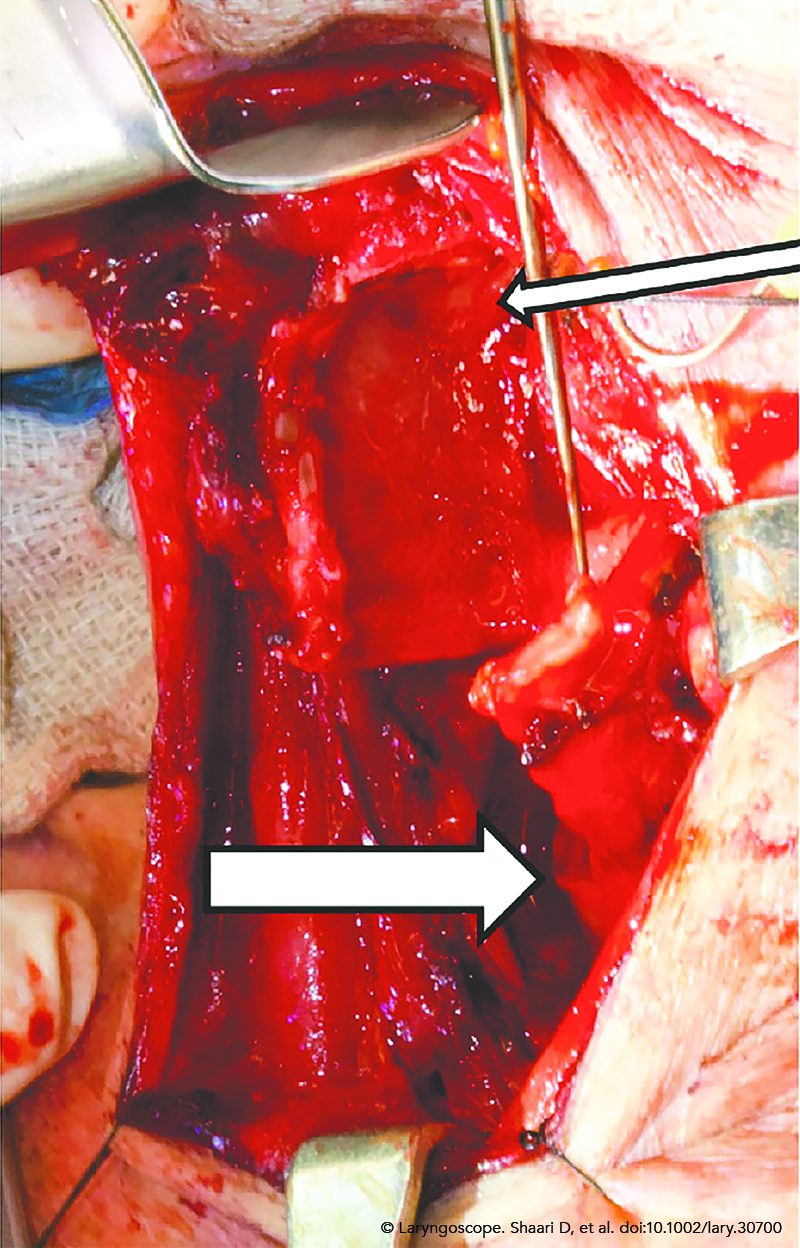
Figure 1. Intraoperative photograph showing the resected cricotracheal segment (small arrow) and ipsilateral hemitracheal ring being advanced to reconstruct the laryngotracheal defect (large arrow).
A 70-year-old otherwise healthy male presented with recurrent papillary thyroid carcinoma (PTC). He was previously treated at an outside institution eight years ago when he presented with hoarseness and was found to have a left true vocal fold paralysis and a mass in the left thyroid and right lateral neck, both of which were positive for PTC. He underwent a total thyroidectomy, a central compartment neck dissection, and a right lateral neck dissection. Pathology demonstrated a 2-cm PTC with extensive extrathyroidal extension into the perithyroidal fat and skeletal muscle. Five lymph nodes were positive without extranodal extension. The patient was treated with 250 mCi of radioactive iodine postoperatively. The left recurrent laryngeal nerve was sacrificed at the time of that initial surgery, and a medialization laryngoplasty was performed. The patient recovered extremely well from that procedure and enjoyed an excellent quality of life with a very active exercise regimen that included cycling and scuba diving.
The patient’s disease remained stable until presentation to our institution eight years later with dysphagia and a rising thyroglobulin level. Imaging showed a lesion within the left tracheoesophageal groove that was inseparable from the cricoid, first tracheal ring, and the esophagus. To treat this recurrence, the patient underwent a cricotracheal resection with a stair-step repair to provide disease control while maintaining airway patency and phonation with reduced risk to the contralateral recurrent laryngeal nerve.
Surgical Method
Positioning and Exposure. The patient was placed in the supine position and intubated transorally with a monitored endotracheal tube. Continuous recurrent laryngeal nerve monitoring was maintained throughout the procedure. The thyroid and cricoid cartilages were skeletonized on the involved side, and the planned hemitracheal and hemicricoid resections were outlined. This resection included the bottom two-thirds of the cricoid from the midline anteriorly to the midline posteriorly and the first two ipsilateral hemitracheal rings. The tumor was also densely adherent to the wall of the esophagus, resulting in a transmural defect, which was closed primarily over a 38 French bougie. Intraoperative frozen resection margins demonstrated clearance of the disease. The third and fourth hemitracheal rings on the normal contralateral side were resected to facilitate cephalad mobilization of the trachea and to minimize damage to the right RLN. A vertical incision was made in the midline of the membranous trachea to complete the removal of those two hemitracheal rings (Figure 1).
Stair-Step Procedure with SCM Flap Bolster. The trachea was advanced superiorly and anastomosed directly to the remaining cricoid without tension using 2–0 PDS sutures. The sutures were left long to facilitate adherence of the SCM to this closure. A superiorly based SCM flap was then harvested by cutting its insertion to the clavicle and it was transposed over the anastomosis. The ends of each anastomotic suture were loaded with a free needle and passed through the SCM and tied. This secured the SCM flap directly over the entire length of the cricotracheal anastomosis with no dead space between the tracheal wall and the undersurface of the muscle.
RESULTS
Pathology showed PTC in peritracheal soft tissue invading cartilage and submucosa with clear surgical margins. The patient was extubated uneventfully on the first postoperative day, with no breathing difficulty throughout the hospitalization. An esophagram on postoperative day seven showed a patent esophagus with no leak. The patient has been able to resume his prior exercise program.