INTRODUCTION
Microtia is mainly characterized by hypoplasia of the auricle, external auditory canal, and middle ear. It usually affects both appearance and hearing. The core of microtia reconstruction is framework fabrication, and an exquisite framework can increase the satisfaction rate and meet the natural aesthetic requirements. (Plast Reconstr Surg. 2014;133(5):1168-1174). In this article, we presented a quantitative framework fabrication technique which mainly needs three rib cartilages. Redesigning the tragus saves the use of cartilage and leaves sufficient concha space for canalplasty. This technique can achieve satisfactory aesthetic results with few complications.
METHODS
Our team has used autologous costal cartilage in microtia reconstruction since 2005. From January 2020 to September 2021, patients with congenital microtia who underwent two-stage microtia reconstruction at a tertiary referral hospital were selected for this study. The first stage is framework fabrication, implantation, and simultaneous lobule rotation, and the second stage is auricular elevation. Some patients need to do the third stage for canalplasty. Our study protocol was approved by the Institutional Board of EYE & ENT Hospital and performed in accordance with the Helsinki Declaration. Patient data were made anonymous for confidentiality. Written informed consent was obtained from each patient.
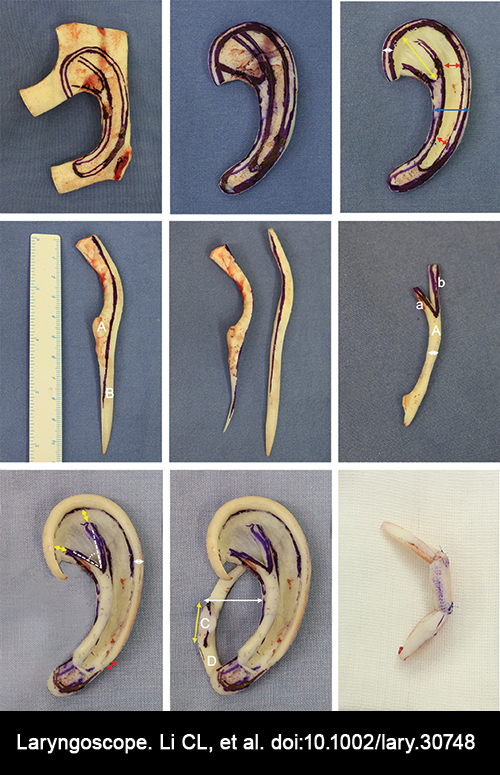
Figure 1. Framework fabrication. (Above, left) Design the base frame on the connected sixth and seventh costal cartilages. (Above, center) Carving the designed base frame. (Above, right) Fabricate the three-dimensional structures like the triangular fossa and scapha. The white arrow shows the outer ring of the frame is 2 mm wide; the blue arrow shows the middle part of the frame is approximately 10 mm wide, the yellow arrow shows the length of the triangular fossa is approximately 15 mm; the red arrow shows the width of the scapha is 4–5 mm at the bottom and widens upward gradually. (Center, left) Design the helix and antihelix structures on the eighth costal cartilage, Part A for the antihelix and Part B for the helix (Center, center). Cut off the designed cartilage. (Center, right) The width ratio between the inferior crura of the antihelix (a) and the superior crura of the antihelix (b) is 1:2. The white arrow shows the antihelix is approximately 2 mm wide. (Below, left) The opening angle of the triangular fossa is approximately 45°; the yellow arrow shows the distance between the tip of the antihelix with the helix is approximately 5 mm; the white arrow shows the width of the helix is approximately 2 mm; the red arrow shows the bottom of the helix structure should reserve 5 mm for connecting to the rotated lobule. (Below, center) Part C is the tragus, which curves slightly. The thickness is 2 mm, the height is 7–8 mm, and the yellow arrow shows the length is approximately 10 mm. Part D is the cartilage piece shoveled from the scapha. The white arrow shows the space of the cavity of the concha is at least 15 mm to accommodate future canalplasty. (Below, right) A C-shaped cartilage stent is fabricated with residual costal cartilage.
Harvesting the Costal Cartilage
We mainly harvest the sixth, seventh, and eighth costal cartilages from the contralateral side. If the harvested cartilage is insufficient for framework fabrication, the ninth or fifth cartilage could be harvested.
The Size of the Framework
The age, height, remnant ear, and skin thickness should be considered when designing the size of the framework. The frame template was created with reference to the opposite ear in unilateral patients and the standard frame template in bilateral patients. The length of the framework needs to be 6 mm shorter than the contralateral side or the expected auricular size. If the remnant ear is too small for lobule rotation, the length of the framework can be increased. The width of the framework needs to be 3–4 mm shorter than the contralateral side or the expected auricular size. Considering future growth, the final ear length should be 2–4 mm longer than expected for adolescents.
The Thickness of the Framework
The maximum thickness of the framework should be <10 mm, and the overall thickness should gradually decrease from top to bottom. The thickness of the base frame should be 3–5 mm, and the helix should also be 3–5 mm. Although a thinner framework could obtain better aesthetic results after auricular elevation, it increases the risk of framework instability.
Base Frame Fabrication
We used Nagata instruments (Medicon, Germany) for framework fabrication. The base frame is the foundation of the framework. Its structural stability and integrity are crucial, and the connected sixth and seventh costal cartilages will increase the stability of the base frame. For quantitative framework fabrication, we first design the base frame on the cartilage, then carve the base frame and fabricate three-dimensional structures such as the triangular fossa and scapha. When we fabricate the scapha, the cartilage should have shoveled integrity, which can be used for tragus fabrication. The outer ring of the frame is 2 mm wide, the middle part of the frame is approximately 10 mm wide, the length of the triangular fossa is approximately 15 mm (approximately a quarter of the ear length), and the width of the scapha is 4–5 mm at the bottom and widens upward gradually.
Helix and Antihelix Fabrication
The helix and antihelix are the crucial aesthetic structures of the framework. For quantitative framework fabrication, the eighth costal cartilage is used for helix and antihelix fabrication. We design the helix and antihelix structures on the cartilage first and then cut off the cartilage. The length of the helix structure is approximately 1.5 times the expected ear length; thus, a minimum of 5 mm overlap could be reached between the helix and the rotated lobule to make the smooth connection. The helix structure is trimmed, and the overall width of the helix is approximately 2 mm. The inferior crura of the antihelix are shaped, and the superior crura of the antihelix are blunted to fit the natural aesthetic. The opening angle of the triangular fossa is approximately 45°, and the distance between the tip of the antihelix and the helix is approximately 5 mm. The helix and antihelix are fixed with a base frame using titanium wire (Taizhou Laser Medical, China) or Prolene suture.
Tragus Fabrication
The tragus is one of the most delicate structures of the framework. Unlike the method of Nagata or Firmin, the tragus is a triangular block that is slightly inwardly curved; the overall length is approximately 10 mm, the thickness is 2 mm, and the height is 7–8 mm. The tragus is fixed with one cartilage piece that shovels integrity from the scapha. From the perspective of specialized plastic surgery, the major concern is that we should reserve a certain space in the cavity of the concha (at least 15 mm) for future canalplasty. Thus, the antitragus and crus of the helix are not the main structures, as they may affect canalplasty. If the residual costal cartilages are sufficient, a C-shaped cartilage stent is fabricated and embedded in the abdomen for the next auricular elevation (Fig. 1). We used the posterior fascial flap technique to do ear elevation. Generally, we do not need to fabricate a tragus for a concha-type microtia.
Evaluation of the Post-Operative Aesthetic Results
Each patient has a dedicated archive to record pre-operative, intra-operative, and post-operative follow-up photographs using the Evernote application. The aesthetic results were all rated as excellent, good, or fair (Plast Reconstr Surg. 2018;141:713-724; Plast Reconstr Surg. 2018;142(1):170-179). An excellent reconstructed ear contains all of the main substructures with natural aesthetics; a good ear contains all of the main substructures, but the natural aesthetics are not good enough; a fair ear contains some major substructures, but some substructures were lost due to infection, deformation, absorption, or displacement, which affected the overall aesthetic results. Two senior doctors who had done more than 1,000 ear reconstruction surgeries (members of the International Society for Auricular Reconstruction) analyzed the aesthetic results and complications of microtia reconstruction at the last follow-up.
RESULTS
A total of 525 patients who underwent two-stage microtia reconstruction with quantitative framework fabrication were reviewed. The average age at first-stage surgery was 10.7 ± 4.0 years (range 7–33 years). There were 379 males and 146 females; 40 patients were bilateral, including 18 patients with bilateral microtia reconstruction simultaneously (Fig. 2), 304 patients were right side, 461 patients were lobule type, and 64 patients were concha type. Hemifacial microsomia was seen in 72 patients, and 13 patients had facial paralysis. The mean follow-up time was 21.4 ± 7.1 months (range 12–33 months).
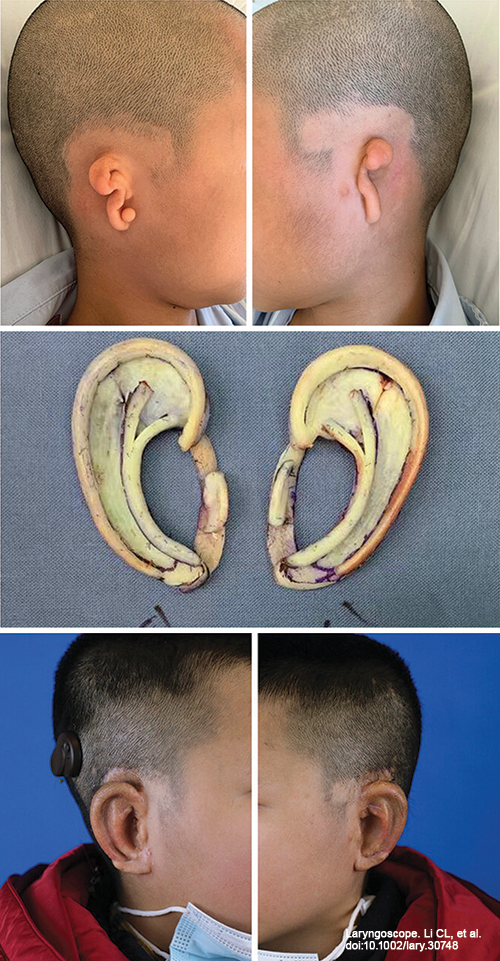
Figure 2. Simultaneous surgical treatment of bilateral microtia. (Above) A 9-year-old boy with bilateral lobule-type microtia. (Center) Bilateral fabricated frameworks at first stage surgery. (Below) Postoperative view after auricular elevation.
In this group of cases, 263 (50.1%) patients obtained excellent reconstructed ears with natural aesthetics; 238 (45.3%) patients obtained good outcomes, and the natural aesthetics were affected mainly due to a shallower scapha, smaller cavity of the concha, unreasonable structural proportions, or mild changes of the substructure; 24 (4.6%) patients obtained fair outcomes, and the main reasons were compression while sleeping, cartilage exposure, framework fracture, and absorption.
Complications occurred in 36 (6.8%) patients, which is lower than in the previous study (12.2%) without quantitative planning (Int J Pediatr Otorhinolaryngol. 2019;116:1-6). There were 11 patients with flap necrosis resulting in cartilage exposure in five patients, framework absorption in 10 patients, mainly due to compression while sleeping, antihelix absorption in five patients due to suture reaction, and tragus absorption in two patients due to weak fixation. Helix displacement occurred in three patients due to compression while sleeping. Helix fracture occurred in three older male patients (27, 32, and 33 years old), and their costal cartilage was partially calcified. Post-operative hematoma occurred in one patient due to incomplete hemostasis. Framework infection occurred in one patient who had undergone an unsuccessful meatoplasty 10 years ago, and the ear canal had atresia just one month prior.