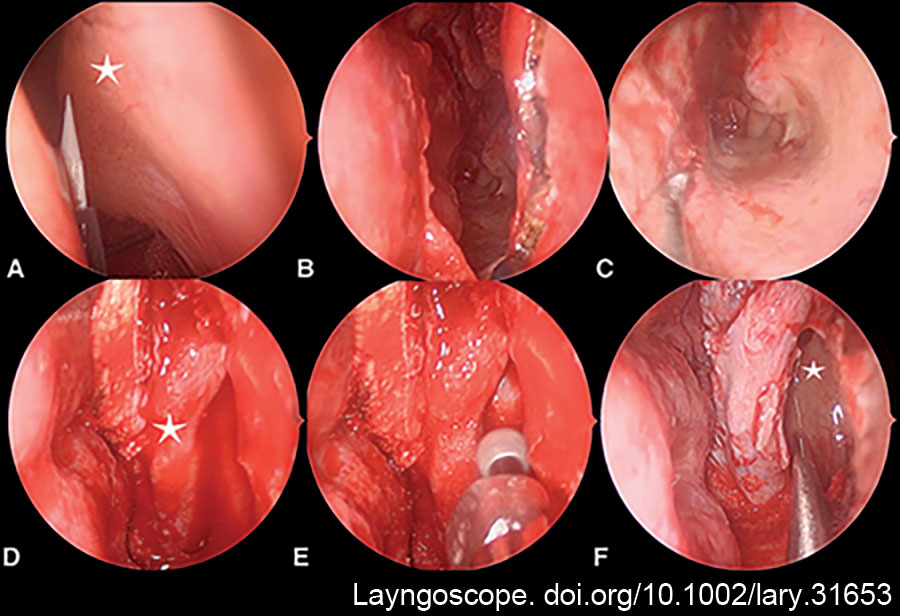
FIGURE 1: Prelacrimal approach steps. Representative intra-operative endoscopic imaging of the left nasal cavity. (A) Lateral nasal wall incision high above the axilla (star) near the nasal roof. (B) The incision carries forward to the bony pyriform aperture. (C) The incision carries down to the nasal floor and medially to the nasal septum. (D) Nasolacrimal duct (star) is mobilized and preserved. (E,F) A prelacrimal window is created using a 4-mm 15° diamond burr, and the posterior maxillary wall (star) is accessed using a 0° endoscope.
The posterior wall of the maxillary sinus can be accessed through this perilacrimal corridor, and mucosa from the posterior wall is marked with a diathermy and taken down. The bony back wall of the posterior maxillary sinus is then removed medial to the infraorbital nerve with a Kerrison rongeur. The fascia over the pterygopalatine fossa contents is cauterized with bipolar electrocautery, and the internal maxillary artery is dissected and either mobilized away from the field of view or ligated with medium endoscopic clips via a 5-mm laparoscopic clip applicator (Ligamax 5MM Endoscopic Multiple Clip Applier, Ethicon, N.J.) and divided. The periosteum over the pterygoid process is elevated, and the pterygoid process is drilled with a 4-mm 15° diamond burr (IPC, Medtronic, Fla.) lateral to the sphenopalatine foramen, Vidian canal, and medial to the infraorbital nerve. Direct access to the lateral sphenoid recess is then achieved with a 0° endoscope. The underlying pathology is then able to be addressed, and multilayer reconstruction is achieved through this access. Our preference is to preserve the lateral recess and remove mucosa only immediately around the defect to receive a limited mucosal graft. If the lateral recess is to be obliterated, then the entire mucosa is stripped and drilled, the space is obliterated with gelatin foam, and the mucosal graft is used on the posterior maxillary wall.
Explore This Issue
December 2024In closure, Gelfoam (Pfizer, N.Y.) is placed in the lateral sphenoid recess, and the inferior turbinate mucosa is returned with three to four sutures (5/0 Vicryl-Rapide, Ethicon, N.J.). The septum is covered with two 0.5-mm silastic sheets (Medtronic, Fla.) and secured with suture (4/0 Prolene, Ethicon, N.J.). The middle meatus is stented with either absorbable or nonabsorbable material. In all cases, image guidance was not used. The entire operation is performed with a 0° endoscope and straight instruments, including bipolar cautery.
Post-Operative Care
Patients were kept in hospital for neuromonitoring following surgery for two to five days. Amoxicillin/clavulanic acid was given for 10 days, and prednisone was given at 25 mg daily for seven to 14 days to reduce congestion and swelling. Nasal saline irrigations were commenced on discharge and delivered as 240 mL twice daily. Patients were followed up at three weeks post-operatively for removal of the silastic sheets and again at three months for review of the neosinus cavity.
RESULTS
Six patients (41.5 ± 9 years, 50% female) were assessed. Follow-up was 50.1 ± 25.2 months. All patients had defects lateral to the V2 nerve and were successfully treated using the PTMA without the need for revision surgery. Five out of six patients had left-sided pathology. Two patients (33%) had previous surgery at another institution and presented with ongoing CSF rhinorrhoea; one was revision surgery for ongoing CSF rhinorrhoea with a defect in the lateral sphenoid recess, and one patient had a left-sided encephalocele in the lateral sphenoid recess. No patient had a lumbar drain inserted during the recovery period.
Two patients (33%) reported temporary paraesthesia along/in the V2 distribution, which resolved after 90 days. No other early or late morbidities were seen.