INTRODUCTION
Pierre Robin sequence (PRS) has an estimated prevalence of one in 10,000 births and is characterized by micrognathia and glossoptosis leading to upper airway compromise. An additional characteristic is a U-shaped cleft palate and feeding difficulties. As airway obstruction can be life-threatening, immediate recognition and treatment are vital. Different surgical and nonsurgical treatment options are available. Initial nonsurgical treatment options include prone positioning, nasopharyngeal airways, palatal plates, and continuous or intermittent positive airway pressure. Surgical treatment options are tongue–lip adhesion, mandibular traction, subperiosteal release of the floor of the mouth, mandibular distraction osteogenesis, and tracheostomy (JAMA Pediatr. 2016;170:894-902. Cleft Palate-Craniofacial J. 2003;40:180-185). Prior to surgical interventions, the multidisciplinary team might consider noninvasive options such as pre-epiglottic baton plate, which demonstrated efficacy in a randomized controlled trial (J Pediatr. 2007;151:145-149). We demonstrate the workflow and practical steps to relieve upper airway obstruction, facilitate feeding, and support mandibular catch-up growth with a pre-epiglottic baton plate in patients with PRS.
Explore This Issue
August 2024CASE EXAMPLES/METHODS
This study was approved by the Ethics Committee Northwest and Central Switzerland (Project ID 2021-01988). Parental consent was obtained for footage material and pictures.
A newborn female presented with respiratory distress with inspiratory stertor and suprasternal retractions immediately after spontaneous delivery. In the supine position, she showed desaturation with oxygen saturation (SpO2) below 90%. In a prone position, the newborn did not require any respiratory support. Physical examination showed mandibular hypoplasia and retrognathia. Oral inspection revealed posterior displaced tongue (glossoptosis) interposed to the backside of a U-shaped cleft palate. Due to feeding difficulties, nasogastric tube feeding was initiated.
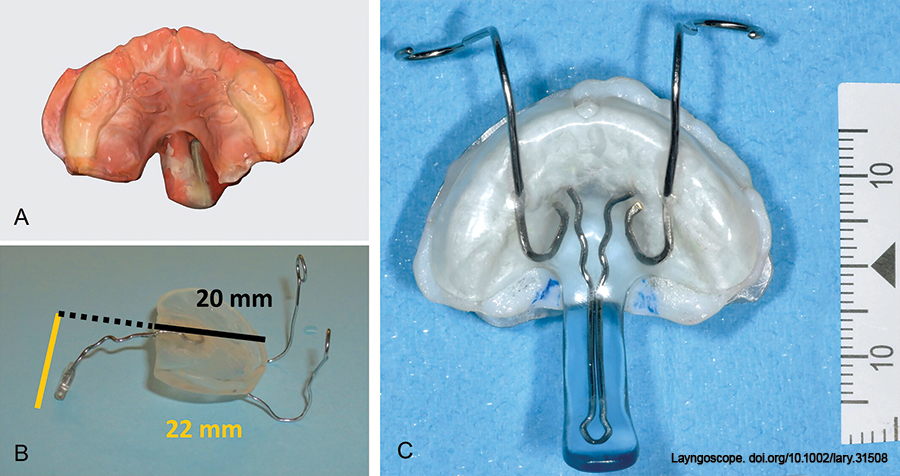
Figure 1: Digital model (A), obtained by a digital intraoral scanner, showing a U-shaped cleft palate, pressure sores of the tongue on the vomer, and nasogastric feeding tube on the left side. (B) Pre-epiglottic baton plate prefabricated with a wire (0.9 mm) connecting the base and pre-epiglottic baton with measurements depicting the anteroposterior length of the plate to the start of the wire (black) and the craniocaudal length of the wire with the pre-epiglottic baton (yellow). (C) 3D-printed model of the palate with corresponding plate where the pre-epiglottic baton was reinforced with resin after the correct 3D positioning was determined.
Due to the risk associated with conventional dental impressions in patients with Robin sequence, we performed a digital impression with an intraoral scanner on the awake patient (Fig. 1A; Medit i500, Medit Corp, Seoul, South Korea). The digital model was then sent for three-dimensional (3D) printing, and a dental technician fabricated a resin pre-epiglottic baton attached with a wire (0.9 mm diameter) to the base of the palatal plate. As a rule of thumb, in the first prototype, the length of the plate (alveolar process to tuberosity) is approximately equal to the craniocaudal length of the wire with the pre-epiglottic baton (Fig. 1B). A resin baton a few millimeters longer may be used. It can be shortened by grinding, depending on the clinical findings (gag reflex, resistance to insertion). The wire allows for further customization by bending the ideal curvature to provide optimal tongue base pressure, relieve airway obstruction, and allow oral feeding. A SpecialNeeds Feeder (Medela AG, Baar, Switzerland) is used for feeding. In the first days, the wire allows further adjustments, and, only when the plate and baton morphology have proven to be appropriate, the wire might be reinforced with resin to fix the position (Fig. 1C). Extraoral wire extensions are necessary for counterpressure and are fixed to the forehead using rubber bands.
The accuracy of the palatal plate to the upper jaw and the position of the pre-epiglottic baton is checked primarily in the clinic. The wire connecting the palatal base to the pre-epiglottic baton is used to adjust the sagittal curvature but also the length (by inserting S-curves or alternatively shortening the baton by grinding). In the case of stable breathing without stertor or gagging in the supine position, the function during feeding must be observed. Fiber endoscopic position verification of the baton for fine adjustment is performed on the awake child as a supplement. Fiberoptic controlled adjustment of the pre-epiglottic baton plate is especially important in children who have already been intubated before attempting to extubate. Parents are instructed in plate removal and insertion for once daily cleaning and disinfection of the plate.
RESULTS
In this case, as a result of the treatment, the newborn could be placed in a supine position again without desaturation and was bottle-fed.
On day 18, the nasogastric tube was removed, and the newborn was discharged three days later for outpatient treatment. Follow-up at two months showed normal thrive (25th percentile) with bottle feeding. A new appliance was needed at around eight to 12 weeks of age, and then at around six months, to accommodate growth. By the ninth month, plate therapy was discontinued with no respiratory or feeding problems. No surgical intervention was required, besides the cleft palate repair at 10 months of age, which was uneventful in terms of respiration and healing.