INTRODUCTION
Over the last few years, considerable progress has been achieved in surgical closure of nasal septal perforations (SPs) (Arch Otorhinolaryngol. 2019. doi:10.1007/s00405-019-05490-w). The surgical outcome still largely depends, however, on the size of the SP (Arch Otorhinolaryngol. 2019. doi:10.1007/s00405-019-05490-w). Low efficacy of surgical repair of large SPs resulted in an increasing number of publications dedicated to surgical enlargement of SPs (Facial Plast Surg. 2019. doi:10.1055/s-0038-1676049).
Explore This Issue
March 2024Trying to improve prognosis, I. Alobid proposed an endoscopic extended AEA (EAEA) flap, which increases the area of the elevated flap significantly (Laryngoscope. 2022. doi:10.1002/lary.29748). The posterior septal artery (PSA), which provides the main blood supply of the nasal septum, is transected during the posterior incision and excluded from the EAEA flap supply (Laryngoscope. 2022. doi:10.1002/lary.29748). Based on anatomy, we modified the Alobid’s flap to include branches of PSA in its supply (Head Neck. 2015. doi:10.1002/hed.23775).
This work aims to demonstrate the effectiveness of the endoscopic repair of large SPs utilizing flap pedicled with branches of PSA.
METHOD
Fifty-two patients with SPs were operated on in 2021 by a senior author using a PSA flap. Thirty-nine of the patients were females, while 13 were males. The mean age of patients was 37 years, ranging between 19 and 66 years. Thirty-two patients had iatrogenic SPs. The most common complaints were nasal dryness, crusting, and nasal obstruction.
In most cases, perforations were localized at the anterior and middle portions of the septum. Sizes of perforations ranged from 3 to 40 mm in the sagittal plane and 2 to 25 mm in the vertical plane (with a mean size of 23 x 12 mm).
Twenty-two patients presented large nasal SPs. Among these patients, the number of iatrogenic SPs was 17, which is significantly higher than in the general group. PSA flap was combined with an “inverted edge” technique on the contralateral side (Int J Pediatr Otorhinolaryngol. 2020. doi:10.1016/j.ijporl.2019.109817). Results of surgical treatment were evaluated six to 12 months after surgery, according to two criteria: SNOT-25 and complete closure of perforation.
Surgical Procedure
In cases of perforations with well-epithelized margins, we started with an elevation of the “inverted edge” flap. A fringing incision around the perforation was made with a 15th-blade scalpel. The distance between the incision and perforation margin was about 5 to 7 mm. Then, the mucoperichondrium was sharply elevated toward the perforation using a suction round knife and turned to the contralateral side of the nasal cavity, leaving an “umbo”-like gap at the center of the flap. This gap was sutured with Vicryl 5/0 or Monocryl 5/0. Using this technique, we achieved complete or partial unilateral repair of the SP and created a wide strip of wound surface at the initial side of the septum (Int J Pediatr Otorhinolaryngol. 2020. doi:10.1016/j.ijporl.2019.109817).
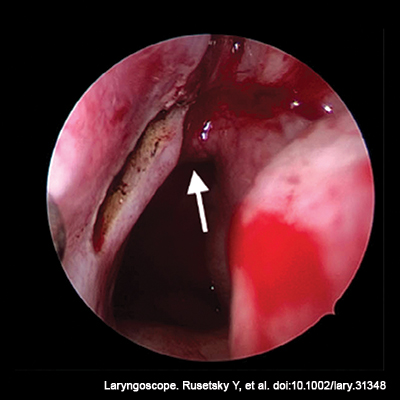
Figure 1. Intraoperative view of the left nasal cavity via a 0° endoscope at the start point of the incision. The arrow indicates the arch of the choana.
To prepare the PSA flap, the posterior incision, made by a bipolar coagulator, started from the posterior end of the middle turbinate (Figure 1), then descended along the posterior edge of the septum obliquely to the border of the hard and soft palate. After that, the incision crossed over the nasal floor and went laterally to the inferior meatus, arising to its lateral wall. Before reaching the lamina of the inferior turbinate, the incision turned anteriorly and went to the axilla of the inferior turbinate. From this point, the incision crossed the nasal floor along the edge of the pyriform aperture, going to the anterior margin of SP. After that, the incision bent around the inferior and posterior edges of the perforation and stopped 5 to 7 mm higher than the posterior border of the perforation.
It is important to note that, in cases of a combination of “inverted edge” and PSA flap, the medial incision of the PSA flap coincides with the incision for the elevation of the inferior part of the inverted edge flap.
Flap dissection can be performed using a round knife or sharp dissector. Flap elevation started from the pyriform aperture and continued along the nasal floor and the septum to the posterior incision. The most challenging point of dissection was the area of the incisive canal. Hemostasis was achieved by using a monopolar coagulator.
Rotation and placing of the elevated flap were performed using soft tip forceps. The flap should cover the whole perforation without any tension. If the tension persisted, the posterior incision continued to the posterior end of the superior turbinate. According to Zhang et al., at this point, the main stem of the posterior septal artery should be situated. We tried not to make an incision higher than 4 mm from the upper edge of the choana because the distance from the arch of the choana to the inferior branch of the posterior septal artery corresponds to 6.72 6 ± 2.64 mm (Head Neck. 2015. doi:10.1002/hed.23775).
The flap was sutured into the edges of the SP, with single knots at the top, front, and bottom (Figs. 1, 4B), usually using Vicryl 5/0 or Monocryl 5/0. To prevent the formation of dead space, contralateral flaps, and PSA flaps were sutured with several transseptal sutures (Vicryl Rapid 5/0).
At the end of the surgery, thorough hemostasis was achieved through coagulation of the donor site. The inferior nasal meatus was tamponaded with Surgicel. Silicone splints were sutured to the columella for two weeks.
RESULTS
The average operating time was 105 ± 42.5 minutes. In all cases, the highest level of the posterior incision did not run more than 4 mm above the choana edge. It preserves the main stem or inferior branch of PSA (6.72 6 ± 2.64 mm, according to Xian Zhang et al.) (Head Neck. 2015. doi:10.1002/hed.23775). There were no cases of postoperative bleeding or other complications. The wound surface of the nasal floor was completely epithelized one month after surgery.
During the postoperative control visit, complete SP closure was found in 48 of 52 patients (92.3%) in the general group, and in 18 of 22 patients (81.8%) of the “large” SP subgroup, which indicates high effectiveness.
