Introduction
Since its initial occurrence in December 2019 in Wuhan, China, the coronavirus disease 19 (COVID-19), caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has rapidly spread worldwide and was officially declared a pandemic by the World Health Organization on March 11, 2020. The surging number of patients who require hospitalization resulted in the temporary transformation of whole hospitals to dedicated COVID-19 centers and massive redeployment of medical personnel to meet the ongoing burden of the pandemic (JAMA Otolaryngol Head Neck Surg. 2020;146:997-998). To combat the pandemic more effectively and to free up hospital resources, cancellation or postponement of all elective operations was recommended, until the epidemiologic situation was more favorable (American College of Surgeons. COVID-19: elective case triage guidelines for surgical care 2020. Accessed online Nov. 5, 2020). This deferral of elective surgery and invasive diagnostic procedures will have a profound impact on patients’ life quality, as some will present with more advanced disease, subsequently leading to more complex surgeries and worse surgical outcomes (Ann Surg. 2020;272:e79-e80). Therefore, diagnostic and surgical procedures had to be modified to maintain the minimum of care for nonurgent and nononcologic patients, principally by introducing personal protective equipment (PPE) and various physical barriers to minimize exposure to potentially virus-containing droplets and aerosol particles in the operative theater (JAMA Otolaryngol Head Neck Surg. 2020;146:671-672; Laryngoscope. 2020;131:956-960). We describe a new technique for the removal of vocal fold polyp in the office setting, while simultaneously taking into consideration the safety measures proposed for the ambulatory examination of the larynx.
Explore This Issue
July 2021Method
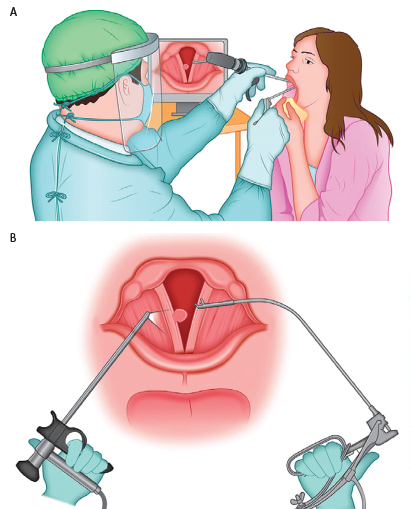
Figure 1. A) Operative setting for the procedure. The surgeon, wearing personal protective equipment, is observing the procedure on the monitor, maintaining adequate distance from the patient. The patient is seated as for routine otolaryngologic examination and is holding the tongue in a gauze. B) Schematics of the procedure. Curved microforceps for indirect laryngeal operations, held in the surgeon’s right hand, is aiming for the lesion of the right vocal fold, under the visual guidance of the rigid telelaryngoscope held in the surgeon’s left hand.
© Ognjen Cukic, MD. Laryngoscope. doi:10.1002/lary.29615
In June 2020, a 74-year-old male patient was seen at our outpatient service for a year-long history of persistent hoarseness. He was a nonsmoker, and, apart from hypertension, his other relevant medical history was unremarkable. Mirror laryngoscopy revealed a well-defined and pedunculated polypoid lesion measuring 4 mm in diameter, originating on the mid-membranous right vocal fold. The mobility of the vocal folds was normal, and the rest of the clinical examination was unremarkable. The preoperative voice acoustic analysis demonstrated jitter, shimmer, and harmonics-to-noise ratio (HNR) values of 0.611%, 7.563%, and 0.0716, respectively. Given the benign clinical characteristics of the lesion and the complete halt of inpatient surgical procedures at our otolaryngology department at the moment of his visit, the possibility of indefinite delay in treatment was presented to the patient. As an alternative, the patient was offered removal of the vocal fold polyp in the office setting using local anesthesia with a negative SARS-CoV-2 reverse transcription-polymerase chain reaction (RT-PCR) screening swab test performed no more than 72 hours before the procedure. On the following visit, the 10% lidocaine solution was applied topically by spraying the oropharynx, epiglottis with laryngeal inlet, and the vocal folds. Following anesthetization, the patient was instructed to hold his tongue with a piece of gauze, as for mirror laryngoscopy examination. Under the visual guidance afforded by the rigid 70° 6-mm telelaryngoscope held in the surgeon’s left hand and attached to the wireless camera and the cold light source, the Brunnings cup forceps attached to the instrument for indirect laryngeal operations held in the right hand was introduced in the patient’s oropharynx (Figure 1). While observing the endolarynx on the monitor, the vocal fold polyp was grasped by the forceps and subsequently removed in a single anterior to posterior motion, respecting the layered histological structure of the vocal fold. (See the supporting video.) The patient was discharged immediately after the operation, with nothing-by-mouth advice for another hour following surgery to avoid aspiration. Complete voice rest was recommended for the next 48 hours, and the patient was instructed to have alternative means of communication at hand (pen and piece of paper, text messaging by cell phone, etc.). No medications were prescribed postoperatively.
While observing the endolarynx on the monitor, the vocal fold polyp was grasped by the forceps and subsequently removed in a single anterior to posterior motion.
The use of this surgical procedure has been approved by the Institutional Ethics Board of the Clinical Hospital Center Zemun from March 19, 2020, under reference number 109/1.
Results
The voice improvement was observed immediately during the surgery, after removal of vocal fold mass which interfered with glottal closure during the phonation. The postoperative acoustic analysis demonstrated improvement in the measured parameters, with jitter, shimmer, and HNR values of 0.215%, 5.991%, and 0.0392, respectively.