INTRODUCTION
Oroantral fistula (OAF) and oronasal fistula (ONF) are related conditions that describe an abnormal, epithelialized communication between the oral cavity and the maxillary sinus or nasal cavity, respectively. Patients present with bothersome reflux of oral contents (e.g., saliva, food) into the nasal cavity during deglutition. There are numerous factors that can lead to the development of a fistula, such as dental extractions, tumor resection, osteonecrosis secondary to radiation and medications, and trauma, among others. Small fistulas may close spontaneously, but the persistent fistula may be a difficult problem to address surgically. Commonly employed techniques for fistula closure include local intraoral flaps (e.g., palatal island flaps, buccal fat and mucosal advancement, facial artery musculomucosal flaps) (J Korean Assoc Oral Maxillofac Surg. 2020;46:58–65).
An alternative, or adjunct, to OAF–ONF repair is using a vascularized, pedicled intranasal flap, such as the nasoseptal flap (Laryngoscope. 2006;116:1882–1886) (NSF) or lateral nasal wall flap (Int Forum Allergy Rhinol. 2020;10:673–678) (LNWF). The NSF and LNWF are pedicled flaps of the posterior septal artery and inferior turbinate tributaries, which are both terminal branches of the sphenopalatine artery and are frequently used in skull base reconstruction. In the current study, we describe a multilayered repair technique for OAF–ONF involving an intraoral local tissue flap combined with a pedicled intranasal flap, with excellent outcomes (see supporting video).
METHOD
Case Series
The first patient is an 85-year-old male with a one-year history of regurgitation of fluids into the right nasal cavity. He was found to have a 1.0-cm right ONF. This was believed to be due to bisphosphonate-related osteochemonecrosis of the maxilla. The patient underwent successful surgical closure of the fistula via a multilayered approach, including right NSF and a left palatal rotational flap.
The second patient is a 64-year-old male with an eight-year history of a right OAF after extraction of right maxillary molars. Shortly after, he developed nasal regurgitation and recurrent right-sided sinus infections. Exam demonstrated a 1.1-cm right OAF adjacent to the location of the first right maxillary molar, and thick mucus emanating from the right middle meatus suggestive of odontogenic sinusitis. He underwent surgical closure, which entailed a right endoscopic medial maxillectomy to treat the sinus inflammation, remove diseased mucosa surrounding the defect, and gain access to the fistula along the maxillary sinus floor. Using a right LNWF to cover the defect from above and a right buccal fat pad flap for intraoral coverage, successful closure, and resolution of symptoms (including sinus infections) were accomplished.
Surgical Technique
Nasoseptal Flap. Initially, the ipsilateral middle turbinate is lateralized, exposing the superior turbinate and posterior septum (Laryngoscope. 2006;116:1882–1886). The natural ostium of the sphenoid sinus is identified posterior to the inferior one-third of the superior turbinate. The flap is harvested using a needle-tip monopolar cautery. The superior cut is made along the posterior septum starting at the level of the sphenoid ostium. Special attention is taken to preserve the olfactory strip superiorly. Depending on the size of the fistula, the flap can be extended anteriorly to the mucocutaneous junction and superiorly to the superior nasal vault. The inferior incision is made immediately above the choana and carried anteriorly to join the previously made anterior incision. Similarly, the flap can be carried laterally off the septum and onto the nasal floor, and even to the inferolateral nasal wall (J Neurol Surg Part B: Skull Base. 2013;74:369–385). Once the perimeter of the flap has been incised, a blunt instrument such as a Freer elevator is utilized to elevate it both off the septum and nasal floor in the submucoperichondrial and submucoperiosteal plane, and stored for later use in the nasopharynx.
Lateral Nasal Wall Flap. An incision is made at the piriform aperture along the ipsilateral mucocutaneous junction and a submucoperiosteal plane elevated along the superior lateral nasal wall, inferior turbinate, and nasal floor, depending on the size of the defect (Int Forum Allergy Rhinol. 2020;10:673–678). The superior incision is along the superior lateral nasal wall and the anterior, posterior, inferior, and lateral incisions over the nasal floor. The flap remains pedicled posteriorly along the posterior aspect of the inferior turbinate. The bone of the inferior turbinate is removed as much as possible and the natural fold of the inferior turbinate is released. The nasolacrimal duct is elevated within the lateral nasal wall mucosa and sharply transected. The exposed bony lateral nasal wall over the flap donor site can then be removed as part of an endoscopic medial maxillectomy anteriorly to the piriform aperture and inferiorly to the nasal floor. The flap may be preserved in the nasopharynx for later use.
Wound Bed Preparation and Flap Insetting. Prior to placement of the flap, on both the oral and nasal sides, the fistula is debrided of diseased mucosa and bone until an adequate margin of healthy tissue surrounds the site. The intranasal flap is then rotated into position to close the fistula from above, and full coverage can be determined from the oral cavity. Angled endoscopes are helpful in evaluating insetting. Intraoral coverage may be performed using a variety of local intraoral flaps, with a palatal island flap used in one of our patients, and a buccal fat pad flap combined with a buccal mucosal advancement flap in the other.
RESULTS
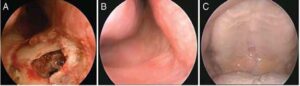
Multilayered repair of OAF–ONF using a pedicled intranasal flap combined with an intraoral local flap facilitated excellent closure in both patients. All procedures were completed on an outpatient basis without complications. Postoperative crusting was debrided in the clinic, which resolved any symptoms related to nasal obstruction. At last follow-up for each patient, the fistulae remained closed with well-integrated, healthy tissue (Figure 1, below). In addition, nasal regurgitation was resolved in both patients.