be distal).
Explore This Issue
November 2024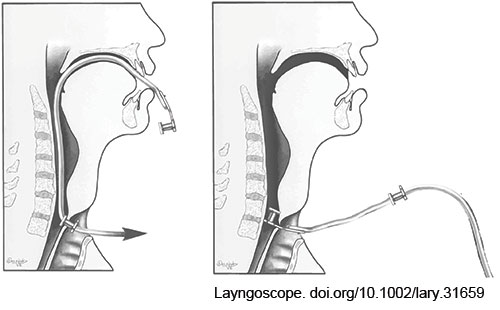
FIGURE 1: Modified retrograde prosthesis placement technique. After passing the catheter through the existing prosthesis in the TEP tract and delivering the tip up through the patient’s mouth, the new prosthesis is secured to the catheter tip and pulled retrograde down the neopharynx and into the TEP tract.
The preexisting prosthesis is now pulled from the tract over the placed red rubber catheter. The new prosthesis can now be delivered in a retrograde fashion by pulling the red rubber catheter back out of the tracheal aspect of the TEP tract (Fig. 1). This will deliver the end of the catheter and the tab of the prosthesis through the tract and into the stoma. Suctioning of mucus or secretions during this process may be necessary. Once the tab of the new prosthesis is visible from the tracheal side of the TEP tract, it is grasped with a hemostat. Another curved hemostat is then used to gently grasp the edges of the tracheal flange of the new prosthesis, adjusting the flange until its entire circumference is freed from the tract. The silk suture connecting the red rubber catheter is cut, and the catheter is discarded.
The new prosthesis is now checked to confirm the appropriate position and function. The prosthesis should rotate easily using a hemostat, confirming that the esophageal flange is properly oriented. The patient is instructed to manually occlude their stoma and phonate to confirm satisfactory function. If rotation is not possible and phonation unsuccessful, this may be due to entrapment of the esophageal flange within the tract, and a longer prosthesis may
be necessary.
RESULTS
Because of the referral nature of our practice, we use this retrograde technique two to four times per month, with 20 retrograde placements in the past year. Three (15%) of these placements were in patients with flap reconstruction, 12 (60%) in patients with a history of esophageal strictures requiring dilation, and two (10%) in patients with a history of stomal stenosis. We have had no complications, and this technique has been successful in all cases where the preexisting prosthesis can be oriented superiorly. We do not use this technique if the preexisting prosthesis cannot be oriented in this fashion.