INTRODUCTION
In recent years, endoscopic medial maxillectomy has been widely adopted for sinonasal tumors; however, traditional medial maxillectomy is required for malignant tumors extending beyond the sinonasal region with involvement of the bony wall of the maxillary sinus or invasion of the orbit. In medial maxillectomy via a lateral rhinotomy, after cutting the medial palpebral ligament (MPL), the inner canthus is retracted laterally with the lacrimal sac, and the orbital contents are protected. Therefore, proper repair of the anterior limb of the MPL is extremely critical for preventing post-operative inner canthus malposition.
MATERIALS AND METHODS
We retrospectively reviewed seven cases of sinonasal malignancy with MPL-repairing surgery attempted with a uniform surgical technique from 2018 to 2023. Institutional Review Board approval for data collection and analysis of medical records was obtained (approved number 2487-16). The mean inter-inner canthal distance of Japanese males was reported to be 34 mm (range: 28–42 mm). It is normally equivalent to the width of the nasal base. Namely, each inner canthus is symmetrical to the midline of the face. In addition, there is no reported left-right difference in the height of the inner canthus in a healthy adult. In this study, the distance from the midline to the inner canthus and the height of the inner canthus were evaluated for each side one year after surgery. Inner canthus malposition was defined as a left-right difference of 5 mm or more.
SURGICAL TECHNIQUE
We inject solutions containing epinephrine in concentrations of 1:200,000 subcutaneously. The lateral rhinotomy incision begins at the inferior hairline of the eyebrow, proceeds downward along the nasofacial junction, and finally enters the alar-facial groove (Fig. 1A). After exposing the maxilla and frontal bone around the piriform aperture and supraorbital rim, the orbicularis oculi muscle is easily visualized between the exposed bones. By pulling the eyelashes laterally, the MPL stands out in a shallow layer, allowing for easy palpation of the MPL within the orbicularis oculi muscle (Fig. 1B). Dissecting along the orbicularis oculi muscle, we can identify the angular vein of the facial vein crossing the MPL (Fig. 1C). At this point, it is important to use skin hooks to pull the skin outward and keep sufficient tension in the surgical field. The angular vein has many branches in this area. All vessels should be ligated carefully. The anterior limb of the MPL, which is identified just below the angular vein, is cut after tagging (Fig. 1D). The medial end of the MPL, which is attached to the anterior lacrimal crest, migrates to the periosteum of the frontal process of the maxilla. The tendon is detached from the anterior lacrimal crest along with the periosteum; they are preserved with allowance for a repair suture. Horner’s muscle and the medial check ligament are detached at the posterior lacrimal crest. The orbital periosteum is elevated with the entire lacrimal sac. The orbital periosteum is detached posteriorly along the medial orbital wall to expose the lacrimal crest, lamina papyracea, and frontoethmoidal suture. If there is a tumor invasion of the orbital periosteum, the invaded area is resected and reconstructed with fascia lata. Osteotomy during medial maxillectomy is performed as previously reported. If sufficient resection margins can be secured, we will partially drill the nasomaxillary buttress and perform an osteotomy that spares the frontal process of the maxilla and the nasal bone where the tendon and periosteum attach (Fig. 1E). After resection, the anterior rim of the MPL is repositioned and repaired with a ligament-to-ligament suture (Fig. 1F, G). Finally, meticulous skin closure is performed (Fig. 1H).
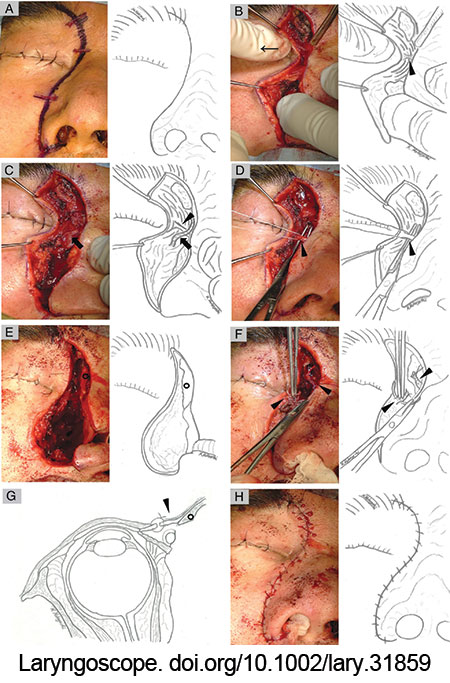
Figure 1: Intra-operative photograph of right medial maxillectomy via lateral rhinotomy. The head was at the top of the photograph. (A) Lateral rhinotomy incision begins at the inferior hairline of the eyebrow. (B) By pulling the eyelashes laterally (thin arrow), the MPL stood out in a shallow layer. (C, D) The anterior limb of the MPL (arrowhead) was identified just below the angular vein (arrow). (E) The osteotomy spared the frontal process of the maxilla and the nasal bone (black circle). (F, G) The anterior rim of the MPL (arrowhead) was repaired with a ligament-to-ligament suture. (H) Skin sutures were formed meticulously.
RESULTS
Pathologically, there were three patients with olfactory neuroblastoma, two patients with human papillomavirus-related multiphenotypic sinonasal carcinoma, one patient with squamous cell carcinoma, and one patient with adenocarcinoma. The primary tumor was resected via a medial maxillectomy in three patients and craniofacial resection with medial maxillectomy in four patients. Medial maxillectomy was performed via a lateral rhinotomy in all patients. Three of the four patients who required craniotomy underwent free flap reconstruction. Three patients required resection of the orbital periosteum and reconstruction with fascia lata. The median follow-up period was 23 months (range, 12–68 months). The MPL was identified in all patients. The median time from skin incision to MPL tagging was 13 min (range, 11–25 min). Ligament-to-ligament suture of the anterior rim of the MPL was achieved in six patients; however, in one patient, the ipsilateral frontal process of the maxilla and nasal bone were completely resected due to tumor invasion; ligament-to-ligament suture of the MPL was difficult. In this case, the lateral cut end of the ligament was sutured to the medial subcutaneous tissue at the same height. All patients underwent surgery as planned, with negative resection margins. The patient with unsuccessful ligament-to-ligament suture of the MPL experienced inner canthus malposition post-operatively (Fig. 2).
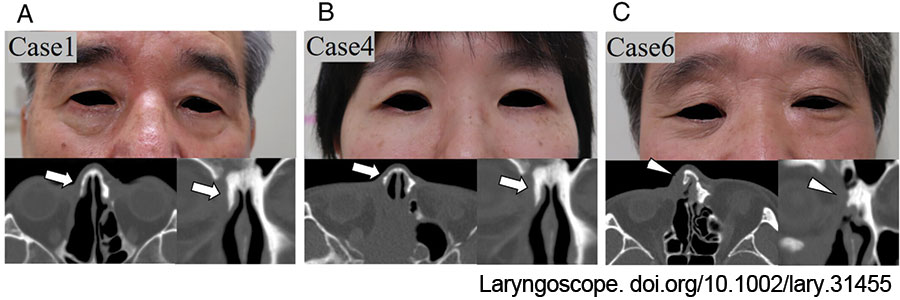
Figure 2: Post-operative facial photographs and CT images. (A, B) Patients 1 and 4 had normal canthal position post-operatively. The frontal process of the maxilla and nasal bone were partially preserved (arrows). The MPL was repaired with a ligament-to-ligament suture. (C) Patient 6 had canthus malposition post-operatively. The ipsilateral frontal process of the maxilla and nasal bone were resected (arrowheads). As a result, ligament-to-ligament suturing of the MPL was unsuccessful. doi.org/10.1002/lary.31859
CONCLUSION
The MPL is easily identified with the eyelash traction test. The angular vein is an anatomical marker. To prevent post-operative canthus malposition, it is important to perform an osteotomy that preserves the frontal process of the maxilla and the nasal bone and to ensure MPL repair with a ligament-to-ligament suture.