 TRIO Best Practice articles are brief, structured reviews designed to provide the busy clinician with a handy outline and reference for day-to-day clinical decision making. The ENTtoday summaries below include the Background and Best Practice sections of the original article. To view the complete Laryngoscope articles free of charge, visit Laryngoscope.
TRIO Best Practice articles are brief, structured reviews designed to provide the busy clinician with a handy outline and reference for day-to-day clinical decision making. The ENTtoday summaries below include the Background and Best Practice sections of the original article. To view the complete Laryngoscope articles free of charge, visit Laryngoscope.
Introduction
Advancements in endoscopic endonasal surgical approaches to the skull base continue to expand; tumors are now resectable through endoscopic approaches that would have previously required transcranial approaches. The nasoseptal flap (NSF) has become the predominant pedicled mucosal flap used in advanced multilayered endoscopic reconstruction to repair skull base defects with cerebral spinal fluid leaks.
Despite its utility, the NSF is not without its complications. It leaves a large, denuded area along the nasal septum that is traditionally allowed to heal by secondary intention, which typically takes 12 weeks. During this time, the lack of functional mucosa and mucociliary clearance allow for the accumulation of dried secretions causing crusting, fullness, anosmia, and a propensity for infection. This necessitates frequent, uncomfortable debridements and causes a decreased quality of life. Additionally, scar contracture from secondary intention increases the risk of septal deformity and saddle nose postoperatively. Placing mucosa along the septal donor site may act as a scaffold, allowing for faster return of mucociliary function and decreased donor site morbidity.
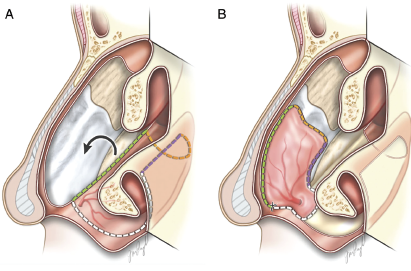
Fig. 1. (A) Illustration depicting the exposed quadrangular cartilage donor site after nasoseptal flap harvest with outline of inferior meatus mucosal flap incisions and counterclockwise rotation. (B) Inferior mucosal flap rotated into position, covering the quadrangular cartilage. Note that the flap covers the superior area next to the nasal dorsum, which is a critical area that can lead to cicatricial contraction and saddle nose if left uncovered.
© Ruffner et. al. Laryngoscope. 2021;131:952-955.
Currently, few options exist for reconstruction of mucosal septal defects. In this study, we describe a novel pedicled rotational flap that uses inferior meatus mucosa pedicled from the greater palatine artery at the incisive foramen (IMF). This flap is harvested on the ipsilateral side of the NSF harvest, and provides ample coverage of the exposed quadrangular cartilage, allowing for more rapid remucosalization and the potential for decreased donor site morbidity. Additionally, it can be used to close existing perforations of the cartilaginous septum.
Method
Four incisions are made to harvest the IMF (Fig. 1). The posterior incision is first performed in the coronal plane from the septum to the tail of the inferior turbinate at the transition between the nasal surface of the soft palate and the nasal floor. The lateral incision is carried along the attachment of the inferior turbinate. The anterior incision is then made along the inferior edge of the nostril at the mucocutaneous junction toward the anterior nasal spine. The medial incision is performed along the transition between the septum and nasal floor. This corresponds to the inferior incision of the NSF. Then the flap is elevated, leaving it attached to the incisive foramen. After harvesting, the IMF is rotated anteriorly and counterclockwise to cover the cartilage of the septum or repair a septal perforation. The flap is then sutured to the caudal septum with 4–0 chromic gut suture in quilting pattern. A Doyle splint is then placed for seven days postoperatively for septal resurfacing after NSF, or 10 to 14 days after septal perforation repair. (See the video link.)
The nasoseptal flap has become the predominant pedicled mucosal flap used in advanced multilayered endoscopic reconstruction to repair skull base defects with cerebral spinal fluid leaks.
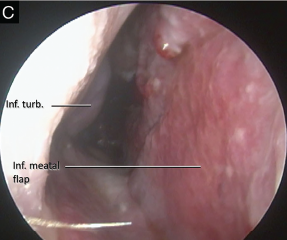
Fig. 2. (C) One month post-operative image showing well healed flap and no evidence of dehiscence.
Results
Six patients had IMF technique in vivo, four patients for resurfacing of the quadrangular cartilage after NSF harvest. The IMF flap covered most of the quadrangular cartilage exposed and reached the nasal dorsum area in all four cases. Mucosalization of the anterior septum appeared complete or near-complete for all patients by one month postoperatively. The flap was also used in two patients for closure of a septal perforation. Patients were followed postoperatively for six months. Both septal perforation repairs were successful. There was no flap necrosis or other permanent complication observed. Transient numbness of the maxillary incisors was present in two patients, both of whom underwent NSF harvest. In both cases, this resolved by the patient’s three-month postoperative visit.
The IMF heals rapidly (Fig. 2). When used for septal perforation repair, the mucosa completely covers the perforation postoperatively and is completely healed one month postoperatively. During NSF resurfacing, the exposed septal cartilage is immediately covered by the IMF. The posterior bony septum and IMF donor site shows signs of granulation at one week postoperatively and near-complete granulation within one month.