INTRODUCTION
Auricular hematomas are a collection of blood between the perichondrium and cartilage or within the cartilage itself. They are commonly caused by blunt trauma and particularly during contact sports (Facial Plast Surgery. 2010;26:451-455). Various treatment options have been described; most involve extracting the hematoma and providing some form of pressure to the area (Laryngoscope. 2012;122:1235-1237). However, a 17-year study showed that recurrence rates were as high as 77% and that even with proper drainage and bolstering, recurrence rates were 14% (Laryngoscope. 2020;130:628-631). Hematomas prevent diffusion to the cartilage, leading to chondritis and potentially the development of cauliflower ear (Facial Plast Surgery. 2010;26:451-455). With this current understanding of the pathophysiology of the sequalae of auricular hematomas, we sought to find a novel surgical approach to manage these recalcitrant cases to prevent this cosmetic deformity.
METHOD
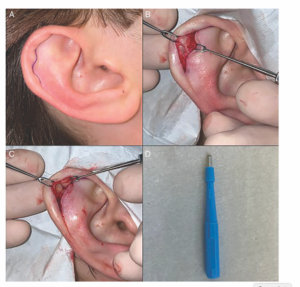
Figure 1. (A) Preoperative view with incision marked. (B) After elevation of the skin, the hematoma coloration can be seen bivalving
the intact cartilage. (C) Demonstration of the bivalve effect on the cartilage. (D) 3-mm hole punch used for this technique
A 19-year-old male was seen after suffering a traumatic auricular hematoma while playing basketball. Two separate attempts of drainage of the hematoma resulted in recurrence soon after each one (Figure 1A). An incision was made along the affected cartilage at the interface of the scapha and helical rim. A skin soft tissue flap was elevated over the affected cartilage. The cartilage was noted to be bivalved by the hematoma (Figure 1B). The anterior layer of the deformed cartilage was excised (Figure 1C). To prevent an additional recurrence, a 3 mm skin punch (Figure 1D) was used to “hole punch” a portion of the remaining layer of cartilage such that, upon closure, there was apposition of the soft tissue of the anterior skin and soft tissue of the posterior ear without intervening cartilage. The incision was closed, and a bolster was applied for five days. He had no recurrence and good improvement of contour at his one-month postoperative visit. He remains “completely normal” at two years’ follow up.
The same technique was applied to a 26-year-old male also seen after several attempts at draining a hematoma, with subsequent recurrence soon after each drainage attempt. An incision was made along the affected cartilage at the interface of the scapha and helical rim. To prevent an additional recurrence, several 3-mm skin punches were used to “hole punch” several areas of the remaining layer of cartilage, creating a “Swiss cheese” appearance. Upon closure there was apposition of the soft tissue of the anterior skin and soft tissue of the posterior ear without intervening cartilage in several different areas of the scapha. The incision was closed, and a bolster was applied for five days. He had no recurrence and good improvement of contour at his six-week postoperative visit.
A 62-year-old female was seen for right-sided chronic seroma/hematoma present for three to four years, previously treated with needle decompression, incision, and drainage with curettage, long-term bolsters, and oral antibiotics. At presentation, she was “pressing out fluid” three to four times a day through a sinus tract through a prior incision and drainage. Again, the same technique was used, in which several 3-mm “hole punches” were created through the diseased cartilage, taking care to place the punches in non-structural areas of the ear, such as the triangular fossa and scaphoid fossa, to preserve the superior anti-helical fold. Again, closure involved apposition of the perichondral envelopes of the anterior skin and posterior skin without intervening cartilage, and a bolster was applied (see supporting video). The bolster was removed after two to three weeks, and the site continued to heal on postoperative days 12 and 25. She had no recurrence and a mild helical rim deformity at her one-year postoperative visit. The helical rim deformity was likely due to the chronicity of the disease process at the time of treatment, involving more extensive cartilage and scar tissue removal to optimally expose the anterior skin perichondral envelope to the posterior skin perichondral envelope.
RESULTS
This hole-punch technique was performed on five recalcitrant (at least two prior drainages with subsequent re-accumulation) post-traumatic recurrent auricular hematomas. Each had open drainage, hole-punching of the cartilage, and xeroform bolster placed for five to 21 days. All patients had excellent results with no additional recurrences, and no patients developed cauliflower deformity.