INTRODUCTION
Congenital isolated H-type tracheoesophageal fistula (TEF) is a rare malformation of the airway that represents less than 5% of congenital TEF. It is characterized by the presence of an isolated TEF without esophageal atresia. The most common location of an H-type fistula is at or above the T2 level, and it is usually repaired using a cervical approach (Pediatr Surg Int. 2016;32:487-491; Pediatr Surg Int. 2021;37:539-547).
Explore This Issue
April 2023Multiple approaches for intraoperative localization have been described to reduce repair time and avoid unnecessary dissection (Pediatr Surg Int. 2016;32:487-491; Pediatr Surg Int. 2021;37:539-547; J Pediatr Surg. 1998;33:1645-1647; J Laparoendosc Adv Surg Tech. 2016;27:1-4). Nonetheless, to the best of our knowledge, this is the first study to report the creation of a loop using a plastic catheter for TEF cannulation. This article is unique in that it presents a step-by-step surgical video to increase awareness of the procedure and assist with reproducibility of the technique.
METHOD
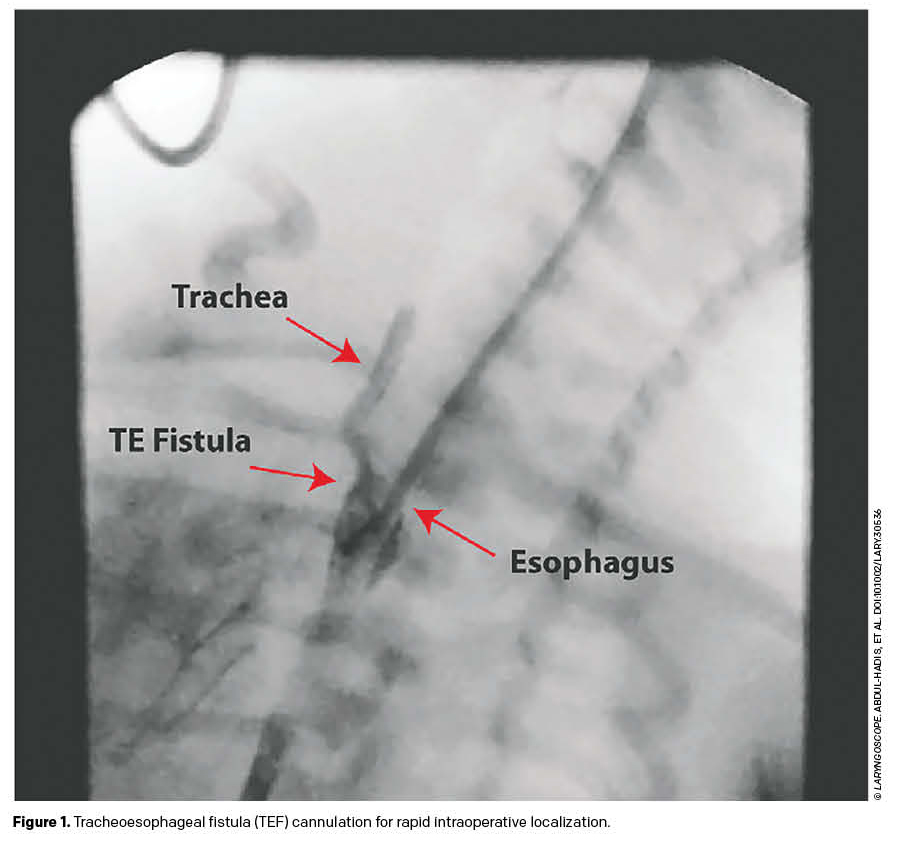 We present the case of a 16-day-old baby boy born at term and adequate for gestational age, who experienced difficulties during his first oral feeds. The patient presented with frequent choking and associated cyanotic episodes, which were unexplained by the diagnosis of unilateral choanal atresia. Feeding through an orogastric tube was attempted; however, the difficulties persisted, and we decided to investigate for an H-type TEF. A fluoroscopic esophageal contrast study was performed, and the findings were consistent with an H-type TEF at the T2 level, approximately 1.5 cm above the carina (Figure 1).
We present the case of a 16-day-old baby boy born at term and adequate for gestational age, who experienced difficulties during his first oral feeds. The patient presented with frequent choking and associated cyanotic episodes, which were unexplained by the diagnosis of unilateral choanal atresia. Feeding through an orogastric tube was attempted; however, the difficulties persisted, and we decided to investigate for an H-type TEF. A fluoroscopic esophageal contrast study was performed, and the findings were consistent with an H-type TEF at the T2 level, approximately 1.5 cm above the carina (Figure 1).
After anesthesia was successfully achieved, the patient was positioned supine on the operating table with a Parsons laryngoscope of the appropriate size in suspension. Airway evaluation was performed under spontaneous ventilation. A 0° rigid endoscope (2.5 mm) was used for the airway evaluation. A TEF was observed, and no secondary airway lesions were identified. A blue whistle tip ureteral catheter was carefully inserted through the posterior wall of the trachea under direct visualization. We were able to leave the catheter in place while simultaneously removing the endoscope. At this stage, the patient was intubated orotracheally and ventilated.
The laryngoscope suspension was released, and rigid esophagoscopy was continued. Once the catheter was identified in the esophageal lumen, it was carefully withdrawn through the mouth to effectively produce a loop from the tracheal side toward the esophageal side of the fistula. The catheter loop was secured using medical tape. Sterile preparation and draping of the patient’s neck was performed, with the head turned to the left.
A horizontal incision was made in the right lower neck, 1 cm above the clavicle. An incision was made using electrocautery, subplatysmal flaps were elevated, and the right sternocleidomastoid muscle (SCM) was identified and retracted. The carotid sheath was then gently retracted. Fistula localization was identified through gentle tugging of the whistle tip catheter loop by the anesthesia team. Dissection of the esophagus was performed circumferentially at the level of the fistula. The esophagus and trachea were adequately discerned, and the recurrent laryngeal nerves were identified and preserved. For retraction, two vessel loops were passed around the esophagus, proximal and distal to the fistula. PDS 4–0 sutures were placed cranially and caudally on the fistulous tract, 2 mm from the trachea toward the esophagus. The looped catheter was then carefully removed by the anesthesia team. The fistula was divided sharply with tissue scissors. The fistula opening was closed with interrupted PDS 4–0 suture.
An SCM muscle flap was placed over the tracheal repair site and secured in place with PDS 4–0 sutures. Subsequently, the esophageal fistula opening was closed transversely using interrupted Vicryl 4–0 sutures. Tracheal closure was confirmed as airtight by filling the surgical site with warm saline, and no evidence of air leakage was noted with positive-pressure ventilation (see supporting video). Hemostasis was maintained. The patient tolerated the procedure well, without complications.
RESULTS
This article provides a detailed demonstration of the steps involved in endoscopic TEF localization and cannulation for rapid intraoperative findings. After confirmation of the H-type TEF diagnosis via fluoroscopy, suspension laryngoscopy and tracheoscopy were used to directly visualize the fistula. A urethral catheter was successfully passed through the fistula into the esophagus. Using rigid esophagoscopy, the catheter was retrieved and withdrawn to form a loop. By applying gentle traction to the catheter loop, rapid intraoperative dissection and localization of the H-type TEF were achieved. The fistula was repaired and an SCM muscle flap was placed over the repair. The patient underwent a normal contrast swallow study postoperatively and subsequently tolerated oral feeding.
Go to https://onlinelibrary.wiley.com/doi/10.1002/lary.30536 to view the video of the technique described here.