INTRODUCTION
Nasal dermoids are uncommon lesions with an incidence of approximately 1:20,000–1:40,000. They can be intranasal or extranasal with or without intracranial extension and are most commonly located on the nasal dorsum (Curr Opin Otolaryngol Head Neck Surg. 2021;29:487-491). The reported incidence of intracranial extension is highly variable, ranging from 4% to 45% (Cleft Palate Craniofac J. 1991;28:87-95). Apart from cosmetic issues and recurrent drainage, nasal dermoids are associated with complications including recurrent infection that may lead to meningitis or brain abscess (Plast Reconstr Surg. 1994;4:745-754). Complete surgical resection is recommended for management, as recurrence is high in incomplete resections with reported rates as high as 100% (Curr Opin Otolaryngol Head Neck Surg. 2021;29:487-491; J Neurosurg Pediatr. 2020;25:298-304).
Traditionally, nasal dermoids with intracranial extension are removed following bicoronal incision and frontal or frontonasal craniotomy (J Neurosurg Pediatr. 2020;25:298-304). This provides great exposure of the dermoid tract; however, it increases the risk of alopecia, unfavorable scarring, meningitis, hyposmia, cerebrospinal fluid leakage, damage to frontal and sagittal sinuses, and other complications related to brain retraction (Curr Opin Otolaryngol Head Neck Surg. 2021;29:487-491; J Neurosurg Pediatr. 2020;25:298-304). Another approach more recently described involved a midline incision with nasal bone osteotomy and keyhole craniotomy (J Neurosurg Pediatr. 2020;25:298-304). Endoscopic approach to resection of dermoid cysts with intracranial extension has also been described. Endoscopic resection virtually eliminates the possibility of unfavorable scarring and other complications associated with craniotomy. Despite the advantages of endoscopy, large intracranial cysts in smaller children are technically challenging to manage due to limited space, which can lead to incomplete resection and potential recurrences (J Neurosurg Pediatr. 2020;25:298-304).
We describe the approach of extended external rhinoplasty with bilateral marginal and alar base incisions, which not only provides access to the nasal part of the dermoid but also excellent visualization of the anterior skull base for complete excision of large intracranial cysts in a cosmetically favorable manner.
METHOD
A retrospective chart review was performed of a three-year-old child presenting with a cystic lesion on the nasal tip that had progressively grown since birth. Computerized tomography (CT) and magnetic resonance imaging (MRI) evaluations showed a non-enhancing anterior nasal lesion measuring 0.9 cm x 0.6 cm x 0.7 cm consistent with dermoid cyst and a sinus tract with a 1-cm intracranial extension.
Surgical Technique
After orotracheal intubation and administration of perioperative antibiotics, the patient’s head was placed in a Mayfield holder. The external nose and nasal septum were injected with 4.0 cc of 1% lidocaine with 1–100,000 epinephrine. Bilateral nasal cavities were decongested with Afrin-soaked pledgets. Frameless stereotactic CT imaging was registered to the patient. Standard rhinoplasty instruments were used for the resection of the intranasal dermoid cyst. An ultrasonic bone aspirator with a barracuda tip was used for intracranial dissection of the dermoid cyst.
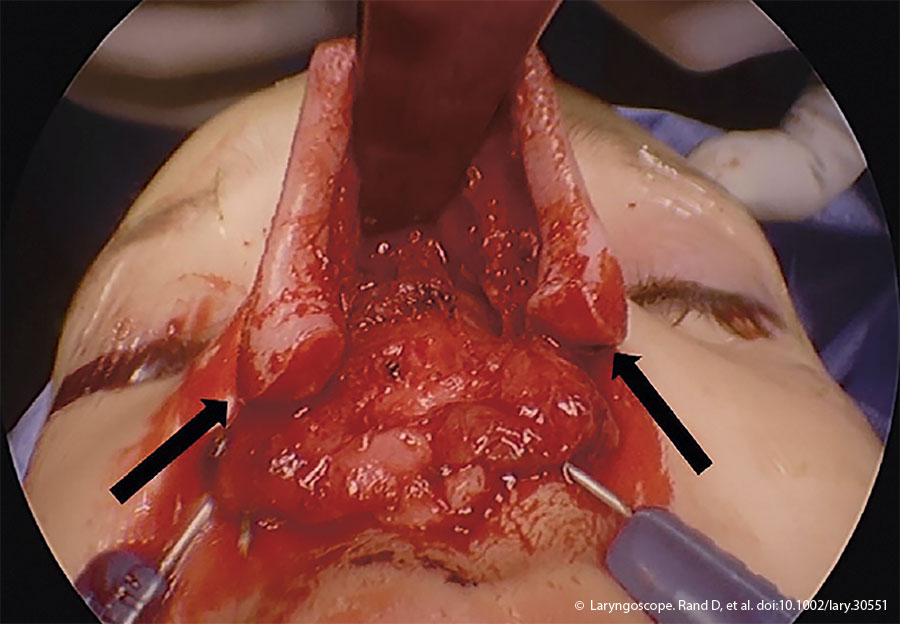
Figure 1. Intraoperative photograph demonstrating the exposure and the alar base extension of the external rhinoplasty incision (black arrows).
An external rhinoplasty approach with an inverted V incision at the mid portion of the columella and marginal incisions was made and extended into alar creases bilaterally. The nasal soft tissue envelope was elevated in a sub-perichondrial plane, and dissection continued over bilateral nasal domes into the lower lateral cartilages. After bisecting the Pitanguay’s ligament, bilateral upper and lateral cartilages were dissected. The incisions were further extended into the alar bases, improving exposure of the nasal dorsum and allowing future access to the anterior skull base (Figure 1). The periosteum was sharply incised over the nasal bones, and a Cottle’s elevator was used to dissect to the radix in a sub-periosteal plane. The dermoid cyst was subsequently dissected from the surrounding soft tissue. A small elliptical excision was required to remove the nasal tip portion of the cyst. Otherwise, the mucosal envelope of the nose was not violated. After transecting the interdomal ligament, bilateral submucoperichondrial flaps were raised from the caudal edges of the nasal septum to the perpendicular plate of the ethmoid bone. The dermoid sinus tract was followed cranially and involved the dorsal septum, which necessitated amputation of the tract and removal of a portion of the quadrilateral cartilage to continue dissection cranially.
Medial and lateral osteotomies were performed with a 3-mm osteotome to remove the left lateral nasal bone, which was placed in saline and set aside. The dermoid sinus tract continued superiorly to the frontal beak and anterior cranial fossa. The nasal dorsum was retracted superiorly to visualize the anterior skull base. The intracranial dissection was achieved by neurosurgery under image guidance. The frontal beak was reduced endoscopically using an ultrasonic bone aspirator. The dermoid cyst was freed from the underlying dura using a combination of sharp and blunt instruments. Complete excision of the cyst was confirmed by visual inspection. The skull base defect was repaired using DuraGen, a resorb X plate, and fibrin sealant. A resorbable plate was used rather than other methods of skull base reconstruction, such as tissue flaps or free grafts, to improve operative efficiency. Nasal reconstruction was achieved. The left nasal bone was replaced in situ and sutured to the piriform aperture and right nasal bone with 3–0 Vicryl sutures. A columellar strut graft fashioned from a piece of conchal cartilage provided tip support. The nasal tip was reapproximated with interdomal sutures with 5–0 PDS suture.
Closure of remaining skin and soft tissue layers was achieved with 4–0 Monocryl sutures reapproximating the dermis and 5–0 fast gut sutures the epidermis. Marginal incisions were closed with 5–0 chromic gut sutures, and the elliptical nasal tip incision was closed with 5–0 fast plain gut chromic sutures. Appropriate dressings were applied. To reduce intracranial pressure postoperatively, a lumbar drain was placed.
RESULTS
Postoperatively, the patient was transferred to the pediatric intensive care unit for monitoring and received perioperative antibiotics. The lumbar drain was removed on postoperative day six. A six-month follow-up showed complete healing, a favorable cosmetic result, and no recurrence on MRI.