INTRODUCTION
Squamous cell carcinoma (SCC) is the most common histologic type of head and neck malignant tumor. Surgery is usually the first choice for the treatment of oral squamous cell carcinoma (OSCC), and, due to the high risk of cervical lymph node (CLN) metastasis in OSCC, a neck dissection (ND) is often carried out.
Conventional open neck dissection (COND) requires a long transcervical incision, leaving a conspicuous neck scar. Varying degrees of esthetic and functional impairments may result from oncologic surgery, either COND or extraoral approach (EOA) of oral cancer resection, which may lead to several psychosocial repercussions and decrease patients’ self-esteem and quality of life. Therefore, minimizing or avoiding facial and cervical skin scars is crucial.
The present study aimed to report our experience and evaluate the feasibility of endoscopic neck dissection (END) through a post-auricular hairline incision (PAHI), followed by intraoral resection of oral cancer and free flap (FF) reconstruction.
METHODS
Study Design and Population
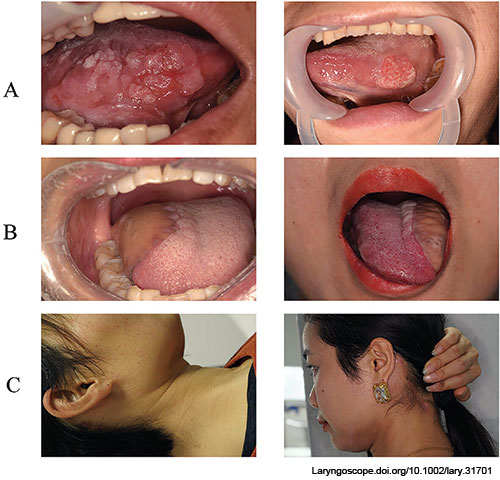
Figure 1. (A) Pre-operative images of tongue squamous cell carcinoma; (B) postoperative images of tongue reconstruction by superficial circumflex iliac artery perforator flap; (C) postoperative images showing no facial and neck scars and the hidden post-auricular hairline scars.
This study included patients treated at the department of head and neck oncology of West China Hospital of Stomatology from November 2022 to December 2023. The inclusion criteria were patients with a confirming diagnosis of T1 or T2 OSCC and clinically negative neck, without a history of prior cancer treatment, without contraindication for reconstructive surgery, without scars of previous lower face and neck surgery or open trauma, age under 60 years, and without distant metastasis. All patients were informed about the possibility of conversion from END to COND, and from intraoral approach (IOA) to EOA. All data were collected prospectively. Patients’ satisfaction was scored as follows: 9-10: very satisfied, 7-8: satisfied, 5-6: average, 3-4: dissatisfied, and 1-2: very dissatisfied.
Surgical Procedures
After general anesthesia and surgical site preparation, an approximately 7 cm PAHI was made. Under endoscopic guidance, the skin-subplatysmal flap was dissected along the surface of the sternocleidomastoid (SCM) muscle, deep to the platysma toward the front, and downward. The dissection extended upward to the surface of the mandible, downward across the level of the intersection of the omohyoid muscle (OHM) and carotid sheath, anteriorly to the submental area, and posteriorly to the posterior edge of the SCM muscle. During skin-subplatysmal flap elevation, the great auricular nerve and external jugular vein were identified and preserved. After the creation of the working space, the SCM muscle was dissected downward beyond the level of the OHM, and the common trunk of the spinal accessory nerve was preserved. When dissecting the deep surface and anterior edge of the SCM muscle, it is necessary to remove part of the lower pole of the parotid gland for good exposure and dissection of level IIb.
The SCM muscle was pulled with a cavity retractor, exposing the range of CLN to dissect above the OHM. The OHM was dissected and exposed, and from the intersection point between the OHM and the internal jugular vein (IJV) (inferior boundary), lymphoadipose tissues (LATs) were dissected upward. From the posterior edge of SCM (posterior boundary), LATs were dissected forward. When using an ultrasonic scalpel to cut or dissect, especially when approaching the carotid sheath, its heat-producing working head should be far from vital structures, such as the IJV, vagus nerve, and carotid artery, among others, to avoid damage. Cervical LATs were then dissected forward and upward from the surface of the carotid sheath to reach the submandibular region, and the facial artery and vein were ligated with vascular clips in patients with tongue SCC and preserved for microvascular anastomosis (MVA) in patients with buccal SCC. Subsequently, the skin-subplatysmal flap was retracted to allow dissection in the submandibular and submental regions (levels Ib and Ia) after the identification of the anterior and posterior bellies of the digastric muscle. The marginal mandibular branch of the facial nerve and SAN was identified and protected. The submandibular gland duct was ligated with a clip and cut into the deep surface of the digastric muscle.
After completing ND, a specimen bag was introduced inside the operating cavity to take out the dissected LAT. The wound was abundantly irrigated, and hemostasis was achieved. A negative pressure tube was placed, and the wound was closed after completing the intraoral procedures.
The tongue and buccal SCC were resected extensively by IOA. The lingual artery and vein were prepared at the remaining tongue for MVA. The facial artery and vein were prepared intraorally in front of the anterior edge of the masseter muscle. Depending on the defect’s size, the superficial circumflex iliac artery perforator (SCIP) flap was harvested. For tongue defect reconstruction, the superficial circumflex iliac artery (SCIA) and lingual artery were anastomosed manually with a 9.0 suture, while the superficial circumflex iliac vein (SCIV) and facial vein were anastomosed with a microvascular anastomotic coupler device (MVACD) using a 1.5-2.5 mm anastomosis ring (AR). For buccal defect reconstruction, the SCIA and facial artery were anastomosed manually with a 9.0 suture, while the SCIV and lingual vein were anastomosed with an MVACD using a 2.0 mm AR. The patency test revealed good blood supply and drainage of the SCIP flap, which was sutured at the defect site. Details on instruments, settings, and surgical procedures are provided in video and supplemental file; other instruments and settings can be found in our previous studies.
Statistical Analysis
SPSS version 26.0 was used for statistical analysis.
Ethical Considerations
Informed consent has been obtained from all patients. The study was approved by the Institutional Review Board of West China Hospital of Stomatology.
RESULTS
This study included eight patients. The mean age was 35.1 ± 10.4 years. There was a female predominance (75%). The tongue SCC represented 75% (Fig. 1) and buccal SCC 25%. T2N0M0 stage accounted for 75% and T1N0M0 stage for 25%. One-team approach and delayed two-team approach accounted for 50% each. All eight cases were reconstructed with SCIP (100%). The mean size AR was 2.1 ± 0.3 mm. The mean intra-operative blood loss was 231.2 ± 96.1 mL. The mean operation duration was 540.4 ± 27.3 min. The mean hospital length of stay was 13.8 ± 1.5 days. The mean follow-up was 8.6 ± 5.4 months. The mean satisfaction score was 9.0 ± 0.5. Pathological analysis of surgical specimens revealed negative margins and no CLN metastasis in all cases; there were no postoperative complications and local recurrence.
CONCLUSION
Both END and IOA of OSCC resection and FF reconstruction have been successfully applied in all our patients. Both techniques were found safe, feasible, minimally invasive, and esthetically appealing options for young patients, resulting in excellent esthetic outcomes and a high degree of patient satisfaction.