INTRODUCTION
Golovine first described the temporoparietal fascia flap (TPFF) in 1898. This flap has been favored due to its resilient reconstructive nature, which surgeons have effectively applied across multiple head and neck subsites. As the thinnest vascularized fascial flap in the human body, its large dimensions and pliability offer reconstructive surgeons a versatile solution. Within the realm of ear reconstruction, an optimal and long-lasting aesthetic result is achieved via a well-defined framework with reliable soft tissue coverage that is thin enough to highlight auricular features (Facial Plast Surg. 2009;25:181–189).
Explore This Issue
July 2023Early alloplastic attempts to recreate the auricular framework utilized various materials that were plagued with an unacceptable incidence of extrusion. Modern microtia repair is performed with a low exposure rate using a porous polyethylene implant enveloped by a TPFF.
Surgical approach via incisions on the hair-bearing scalp, including hemicoronal, S-, Y-, and Z-shaped designs, have been classically described to harvest the TPFF. Incisional alopecia and hypertrophic scarring can make these approaches undesirable in aesthetically-focused cases such as microtia reconstruction. More recently, TPFF harvest through a postauricular incision approach has been described (Facial Plast Surg. 2009;25:181–189). In the authors’ experience, this minimally invasive approach is plausible but can be difficult due to the small and low viewing window. Additionally, this may lead to a higher risk of vascular pedicle injury or inadvertent injury to the frontal branch of the facial nerve. In an effort to facilitate TPFF harvest via a single minimally invasive incision while reducing neurovascular injury risk, this work aims to describe an innovative approach utilizing endoscopic assistance and indocyanine green angiography (ICG).
METHOD
Surgical Technique
General anesthesia and orotracheal intubation are utilized without long-acting paralytic agents to allow visual facial nerve monitoring. The patient is positioned supine with a shoulder roll. Hair over the TPFF can be either braided or shaved per surgeon preference. Standard prep solution and draping are applied. The superficial temporal artery (STA) branches are palpated and marked, as well as the 10 cm width by 13 cm length TPFF. The expected course of the frontal branch is noted. One percent lidocaine with 1:100,000 epinephrine is injected into the postauricular region to facilitate hemostasis. The sole incision is marked following the postauricular curve of the future ear.
 The postauricular incision is made with a 15-blade, and the mastoid skin is reflected anteriorly with concomitant excision of any cartilaginous remnants. Through this sole incision, the entire scalp is carefully elevated from the TPFF in the subcutaneous plane using monopolar electrocautery at 15 watts. The mantra “yellow up, white down” describes the separation of the yellow-colored subcutaneous fat from the white-colored fascial layer below. As dissection proceeds superiorly toward the estimated halfway point between the base of the flap and the anticipated distal point, approximately 7 cm from the start of dissection, concurrent visualization by both surgeon and assistant becomes difficult and the endoscopic portion is initiated. The primary surgeon uses the non-dominant hand to drive a 4-mm, 30-degree Hopkins endoscope loaded onto an Endobrow retractor and holds an extended needle-tip electrocautery device in the other hand. The assistant employs a metal Yankauer suction tip to evacuate surgical plumes and blood and also provides scalp retraction. This technique allows for constant TPFF visualization by both the primary surgeon and the assistant working synergistically. This is particularly helpful when visualization is needed over the curvature of the parietal skull and within the region of the frontal branch of the facial nerve. The previously marked TPFF boundaries guide the final extent of anticipated flap elevation.
The postauricular incision is made with a 15-blade, and the mastoid skin is reflected anteriorly with concomitant excision of any cartilaginous remnants. Through this sole incision, the entire scalp is carefully elevated from the TPFF in the subcutaneous plane using monopolar electrocautery at 15 watts. The mantra “yellow up, white down” describes the separation of the yellow-colored subcutaneous fat from the white-colored fascial layer below. As dissection proceeds superiorly toward the estimated halfway point between the base of the flap and the anticipated distal point, approximately 7 cm from the start of dissection, concurrent visualization by both surgeon and assistant becomes difficult and the endoscopic portion is initiated. The primary surgeon uses the non-dominant hand to drive a 4-mm, 30-degree Hopkins endoscope loaded onto an Endobrow retractor and holds an extended needle-tip electrocautery device in the other hand. The assistant employs a metal Yankauer suction tip to evacuate surgical plumes and blood and also provides scalp retraction. This technique allows for constant TPFF visualization by both the primary surgeon and the assistant working synergistically. This is particularly helpful when visualization is needed over the curvature of the parietal skull and within the region of the frontal branch of the facial nerve. The previously marked TPFF boundaries guide the final extent of anticipated flap elevation.
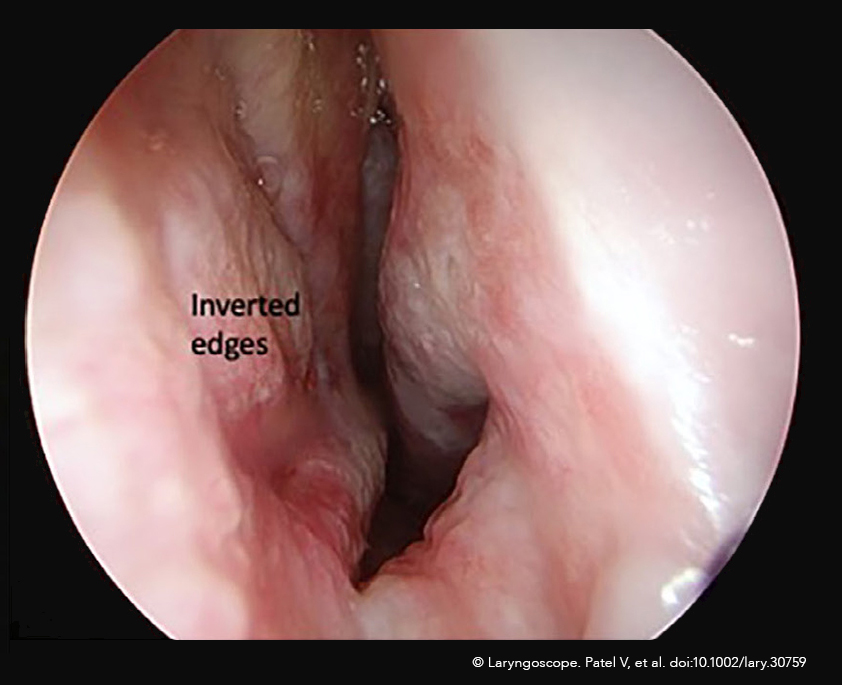
TPFF vascularity is evaluated with an intravenous injection of ICG, a fluorescent dye, before and after harvest to define the arterial anatomy of the STA and to evaluate the vascularity of the flap as it covers the implant, respectively. ICG is administered via a routine peripheral intravenous line at a total dose of 2.5 mg/kg (maximum dose, 25 mg) split between the two administrations. The Rubina 4 K camera system near-infrared fluorescence image overlay function is enabled to perform angiography. Vascular imaging is noted to last approximately 10 minutes after each ICG administration. The first of two ICG angiography runs is performed after subcutaneous scalp dissection but immediately before the TPFF-releasing incision. This critical incision is made immediately anterior to the anterior branch of the STA. The intraoperative angiography greatly facilitates this incision by clearly delineating the STA and its anterior branch (Figure 1, above). Optimal vascular visualization with ICG ensures incorporation of this key vascular pedicle within the flap while keeping the surgeon posterior enough to minimize the risk of injury to the frontal branch of the facial nerve. The TPFF is then released from the deeper layers of the scalp, taking care to bluntly and sharply incorporate the loose areolar layer within the flap. The flap is delivered inferiorly and used to envelop the porous polyethylene implant. Implant assembly is performed as per standard technique; details are beyond the scope of this work. The second ICG angiography run confirms adequate flap perfusion across the entire implant to minimize the risk of postoperative extrusion. Any areas of poor flap vascularity over the implant can be excised, rearranged, or, lastly, covered with pedicled tissue from either the mastoid skin or lobule. A combination of mastoid skin and free full-thickness skin grafts are overlaid to provide cutaneous coverage for the reconstructed ear.
RESULTS
In the authors’ experience, the endoscopic technique paired with ICG angiography facilitates visualization of critical vascular anatomy, which allows for safe TPFF harvest in total auricular reconstruction. For otolaryngologists, the endoscopic technique is intuitive and facilitates TPFF harvest, which is commonly known as the most difficult portion of this challenging procedure. Anecdotally, adoption of the ICG-endoscopic technique has decreased operative times, improved surgeon ergonomics, increased confidence in preserving neurovascular anatomy, and increased resident participation given superior visualization projected onto a 4K screen. A comprehensive investigation of the authors’ results remains ongoing, but the clear early advantage of this technique prompted this group to describe this novel technique in this particular format.