INTRODUCTION
The traditional Draf 2a frontal sinus surgery is challenging due to the complexity and variations of the frontal recess and sinus anatomy (Int Forum Allergy Rhinol. 2017;7:332–337). In particular, the thickness of the nasofrontal beak and anterior–posterior dimensions of the frontal recess make surgery challenging. These limitations affect the ease of Draf 2a surgery (Int Forum Allergy Rhinol. 2017;7:332–337). Several prior techniques have been described to help manage this issue, including an axillary flap, removal of the anterior agger nasi (Laryngoscope. 2002;112:494–499) and an agger nasi punch-out procedure (Laryngoscope. 2006;116:1710–1712). The Carolyn’s window approach aims to remove the limitation created by the anterior–posterior depth to make a Draft 2a frontal sinusotomy easier for the surgeon. The approach is entirely a 0° endoscope technique and provides an excellent view of the frontal sinus and recess.
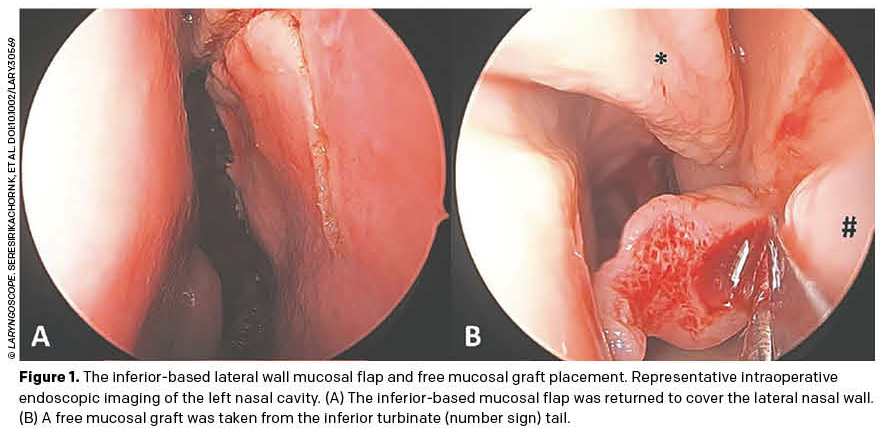
The concept of an “axillectomy,” or removal of the axilla, includes removal of the entire frontal process of the maxilla and nasofrontal beak. This differs from axillotomy, or simply removing the front wall of the agger nasi. The utilization of high-speed powered instruments makes this technique rapid and efficient. The inferior-based lateral wall mucosal flap (modified-Woodworth flap) and free mucosal grafting of any exposed bone make for rapid mucosal healing. After the Carolyn’s window approach, the enlarged middle meatus provides enhanced frontal sinus access and irrigation (Laryngoscope. 2021;131:250–254). We describe the Carolyn’s window approach to frontal sinus surgery and the perioperative outcomes.
METHOD
Outcomes
The primary outcome was frontal sinus patency. Secondary outcomes were surgical morbidity, defined as early (<90 days) or late (>90 days). Early morbidity included bleeding (requiring intervention), pain (requiring additional analgesia), crusting (requiring an additional postop visit), adhesions (any), cerebrospinal fluid leak, periorbital edema or hematoma, and skin changes. Late morbidity included epiphora, smell reduction from baseline, retained frontal recess partitions, and any external cosmetic change.
Preparation
An endotracheal tube was positioned in the lower right commissure. The patient was prepared topically with 1% ropivacaine and 1:2,000 adrenaline-soaked cotton pledgets. Endoscopically, the mucosa was injected with 1% ropivacaine and 1:100,000 adrenaline across the lateral wall anterior to the middle turbinate and the root of the middle turbinate. The patient’s head was at an extended 30°–40°, and the patient was in a 15°–20° reverse Trendelenburg position, with total intravenous anesthesia and bradycardia.
Surgical Technique
A middle meatal antrostomy and at least an anterior ethmoidectomy are performed to identify the medial orbital wall. The approach is often combined with sphenoethmoidectomy or “neo-sinus” or “full-house” surgery. Carolyn’s window commences with the creation of the inferior-based lateral wall mucosal flap (modified-Woodworth flap). The incision on the lateral wall begins at the nasal cavity roof, high above the axilla, by needle-point diathermy, setting 12. The posterior incision, at a depth of the middle turbinate insertion, is carried vertically down to the middle turbinate. The superior incision is carried along the apex of the nasal cavity forward to the pyriform aperture and then vertically down, just behind the pyriform aperture, to a level that approximates the midpoint of the middle meatus. These incisions are to the bone, and the inferior-based lateral wall mucosal flap is elevated subperiosteally, with the flap retracted down and exposing the axilla and lateral wall bone.
Drilling proceeds with a 0° endoscope and a 4-mm 15° diamond burr, at 30,000 revolutions per minute, removing the entire axillaagger nasi-maxillary-frontal process complex. First, the periosteum of the frontal process of the maxilla bone and the nasolacrimal sac are identified as the lateral limits. These were discovered to widen the surgical field. Then, drilling proceeds to remove the entire axilla, lateral to the middle turbinate insertion, but medial to the periosteum that was just defined. Although the first olfactory neuron can be found to define the extent of medial dissection, as commonly performed in a Draf 3, this is generally not required, and the insertion of the middle turbinate serves as the medial landmark. The triangular bone anterior to the frontal recess is removed until the “blue lining” of the mucosa is seen, thus preserving the frontal recess itself. Drilling continues anteriorly and superiorly to remove the nasofrontal beak in a vertical orientation relative to the apex of the frontal sinus. Once the remaining bone is thin, the frontal recess partitions are removed with the 2.5-mm 45° cutting forceps and 4.3-mm quadcut straight microdebrider. The 5-mm 70° Hosemann frontal sinus punch can complete the removal of bone edges but is used with a 0° endoscope. At the end, a giant middle meatus is created with all frontal sinus walls that can be seen through the 0° endoscope.
The inferior-based lateral wall mucosal flap is returned to cover the lateral wall. A free mucosal graft from the inferior turbinate tail is thinned and covers any exposed bone (Figure 1). The middle meatus is stented with hyaluronic acid gel and a Merocel finger glove spacer with no other packing.
Postoperative Care
Spacers were retained for seven to 14 days, and irrigation commenced on the first postoperative day. Patients are managed via day surgery. Amoxicillin/clavulanic acid was given for 10 days, and prednisone was given at 25 mg maximum daily for seven to 21 days to reduce edema/congestion.
RESULTS
Forty-five patients (49.1 ± 17.9 years, 48.9% female) were assessed. All patients had successful frontal sinus patency (100% [95CI: 92.1%–100%]). Follow-up was 39.2 ± 9.0 months. Morbidities were adhesion (4.8%), crusting (2.4%), pain (1.2%), and bleeding (1.2%) in the early postoperative period. There were no other morbidities in the early (cerebrospinal fluid leak, periorbital edema or hematoma, and skin changes) and late (epiphora, smell reduction from baseline, retained frontal recess partitions, and any external cosmetic change) postoperative periods.