INTRODUCTION
Obstructive sleep apnea (OSA) is a chronic disease characterized by recurrent episodes of upper airway collapse and obstruction of the upper airways during sleep. The gold standard of treatment is continuous positive airway pressure (CPAP), with limited long-term patient compliance (Acta Inform Med. 2023;31:96-101). Velopharyngeal surgery is a validated treatment option for OSA patients diagnosed with retro-velar and oropharyngeal collapse.
Explore This Issue
May 2024Vicini first proposed the barbed reposition pharyngoplasty (BRP) technique, using barbed sutures to increase the cross section of the retropalatal area and oropharyngeal inlet, stiffening the pharyngeal lateral wall (Eur Arch Otorhinolaryngol. 2015;272:3065-3070). This mini-invasive technique requires the removal of the “fat pad” area and a section of the palatopharyngeal muscle (PPM) in their inferior portion.
Continuous solicitation of a single vector during palatal activities may weaken the system, inducing a recurrence of pharyngeal collapse. Reoperation is not easy since the PPM has been transected.
Therefore, the authors propose a modified BRP called barbed stayed bridge pharyngoplasty (BSBP).
METHODS
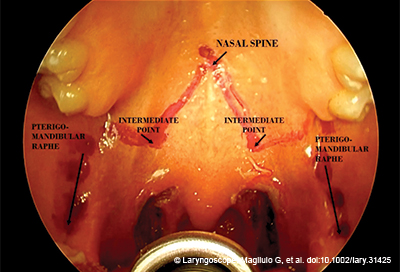
Figure 1. An image from a video demonstrating the BSBP technique, illustrating the landmarks placed in preparation for surgery.
This study was performed at the Organi di Senso Department, Sapienza University of Rome, from January 2022 to May 2023 (Ethical Committee RIF: 6267; principles of the Declaration of Helsinki; informed consent by each patient).
Patients were aged 30 to 60 years, with a BMI ≤35 kg/m2 and no previous ENT surgery or OSA treatment.
The Epworth Sleepiness Scale (ESS) and Home Sleep Apnea Testing (HSAT) type III were administered. OSA grade was based on the apnea-hypopnea index (AHI) and American Academy of Sleep Medicine classification (J Clin Sleep Med. 2017;13:479-504). Moderate OSA patients (pts) were enrolled.
The single-level velopharyngeal collapse was confirmed through a drug-induced sleep endoscopy (DISE).
The patients were classified using the Friedman staging system, excluding stage IV. Only patients graded 0–1 on the lingual tonsil hypertrophy grading system were considered.
Patients had a VOTE (velum, oropharynx, tongue, epiglottis) classification of V1 or 2 concentric/lateral-lateral; O1 or 2; T0; or E0. Anteroposterior collapses were excluded to homogenize the sample.
Otorhinolaryngological (ENT) examination was performed monthly after surgery. HSAT was at three, six, and 12 months postoperatively. The success rate was calculated using the traditional Sher’s cutoff of AHI <20/h and reduction >50%.
Surgical Technique
BSBP is performed under general anesthesia with orotracheal intubation. The patient is placed supine with his head extended (pillow under the shoulders) and a Davis mouth gag applied. Barbed suture Covidien V-Loc 180 Absorbable Wound Closer 3-0 is used, with a thread of 23 cm Green and a taper needle of 1/2 26 mm.
1. Bilateral tonsillectomy is performed, exposing and preserving the PPM and the palatoglossal muscle (PGM).
2. Landmarks are placed using a pen as follows:
• Posterior nasal spine in the midline;
• Pterygomandibular raphe (PMR) divided into three points: superior, middle, and inferior; and
• The intermediate point, located slightly lower along a parasagittal line drawn strictly between the nasal spine and PMR.
3. The needle starts from the posterior nasal spine and continues laterally to an intermediate point. From the intermediate point, it reaches the PMR. The needle tip is extracted from the PMR and inserted into the tonsillar fossa.
4. The margin of PPM and PGM is identified and detached without
any transection.
5. The needle passes longitudinally across the entire PPM as far as its inferior margin. The PGM is not involved.
6. The barbed suture is rolled up the PPM in the inferior part and turned back to the raphe.
7. The same operation is repeated in the middle and superior portions of the PPM and PMR.
8. It reaches the inferior point of the PMR and is rolled up the PPM. The operation is repeated in the middle and superior parts.
9. The needle passes backward lateral to the raphe, applying the right amount of tension to the suture to reposition the PPM more laterally and anteriorly and to splint and tighten the lateral wall.
A senior surgeon performed all procedures (G.M.).
Statistical Analysis
Descriptive statistics were used to summarize the characteristics of the study sample; numerical data were reported as mean with standard deviation.
A comparison between them was performed using Student’s t-test. Statistical significance was set at 0.05. All the analyses were conducted using statistical software R (version 4.0.4).
RESULTS
Ten male patients were enrolled (age = 43.8, ±9.8 years; BMI = 27.2 ± 3.05). Using the Friedman staging system, the authors recorded two pts at stage I, seven pts at stage II, and one pt at stage III. Using the lingual tonsil hypertrophy grading system, the authors recorded four pts at grade 0 and six pts at grade I.
The preoperative mean of ESS was 5.1 ± 3.5; at three months postoperative, it was 3.5 ± 2.6; at six months postoperative, it was 3.1 ± 2.6; and at 12 months postoperative, it was 2.4 ± 1.9. No statistical difference was found.
All preoperative and postoperative polysomnographic data and DISE are in Table I (Laryngoscope. https://doi.org/10.1002/lary.31425).
The comparison between AHI values preoperatively (preop) and postoperatively (three, six, and 12 months) always showed a statistical difference (p < 0.05) using the Student’s t-test. The same was true for the oxygen desaturation index (ODI) comparison, with a p < 0.05, while time under 90% oxygen saturation (t90%) was not statistically significant (p > 0.05)
Sher’s cutoff was successful in all patients (Table I), with an AHI reduction of more than 50% at 12 months; 60% of pts had an AHI < 10 and 40% had an AHI < 5.
The swelling of the palate and uvula was moderate in the postoperative period. The therapy included antibiotics and corticosteroids (prednisolone 40 mg/day/three days; at-home deflazacort 30 mg/day/seven days). Painful symptoms were mild and manageable, with paracetamol 1 g as needed.
No hemorrhagic complications were reported. In three cases, the suture was partially extruded at the palatal level without affecting the procedure’s success. The extrusion was located on the superior pole of the anterior tonsillar pillar, in the first two months. Patients complained of a foreign body sensation and slight swallowing difficulty. The thread was always cut without any long-term effects on the stability of the palate.