Introduction
Since its introduction, endoscopic posterior cricoid split and rib grafting (EPCS/RG) has been performed in patients with subglottic stenosis, posterior glottic stenosis, and bilateral vocal fold paralysis (Laryngoscope. 2017;127:252-257). A challenging step in this procedure, as described by Inglis, et al., is the placement of the cartilage graft into the divided cricoid lamina (Laryngoscope. 2003;113:2004-2009).
We present in this article a modified EPCS/RG that involves the use of balloon dilation to aid in this step of the procedure. It provided additional benefits for older patients. The main outcome measures were the resolution of dyspnea, prevention of aspiration, and need for additional surgeries.
Method
Five patients underwent EPCS/RG with balloon-assisted rib graft placement between October 2017 and April 2021 in King Saud University Medical City. The preoperative patient evaluation included an awake flexible fiberoptic nasolaryngoscopy, pulmonary function test, 24-hour pH study, and swallowing assessment in those with a positive history of choking. Bilateral vocal fold immobility was diagnosed based on the preoperative fiberoptic nasolaryngoscopy, which demonstrated immobilized vocal folds, and the intraoperative confirmation of bilateral passive mobility of the arytenoid joints. Data regarding demographic characteristics, age at the time of EPCS/RG, clinical diagnosis, comorbidities, pre-existing tracheostomies, previous surgical interventions, decannulation outcome, follow-up interval, and resolution of symptoms were obtained.
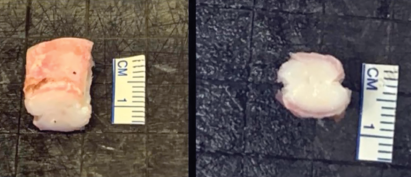
Figure 1. The rib graft is prepared for use by carving a groove on each side.
© Aldriweesh B, et al. Laryngoscope. doi:10.1002/lary.29744
Surgical Technique: The patient is placed under general anesthesia with spontaneous ventilation and insufflation technique. Direct laryngobronchoscopy is performed using a Parsons laryngoscope for younger patients or an anterior commissure laryngoscope with placement of the laryngeal vocal fold spreader in an inverted fashion. Airway examination is performed using a 4-mm, 0-degree Hopkins rod-lens telescope. The arytenoid joints are palpated to check for mobility to rule out associated arytenoid joint fixation. The posterior cricoid plate is locally infiltrated with xylocaine/adrenaline with a concentration ratio of 1:100,000. Endoscopic posterior midline cricoidotomy is performed using the cold steel technique (round or sickle knife) until the entire length of the posterior cricoid lamina is divided. Subsequently, balloon dilation of the cricoid cartilage is performed to allow expansion of the divided cricoid ring. The balloon is positioned to cover the supraglottic, glottic, and subglottic levels; it is inflated for 40 seconds, unless there was desaturation necessitating earlier balloon deflation. The divided cricoid lamina is separated with alligator forceps to assess the space between the divided cricoid ends, which determines the graft width needed. Then, the airway is secured with an endotracheal tube and the laryngoscope is removed.
Since its introduction, endoscopic posterior cricoid split and rib grafting has been performed in patients with subglottic stenosis, posterior glottic stenosis, and bilateral vocal fold paralysis.
Rib graft harvest is performed from the fifth rib. The graft is shaped by carving a groove laterally on each side, and a safety suture (3–0 silk suture) is temporarily applied to the superior part of the graft.
The patient is placed in suspension, and the endotracheal tube is removed to continue the insufflation technique. The graft is placed into the cricoid split with the graft’s perichondrium on the laryngeal lumen side. One side is wedged into the cricoid split. The second balloon dilation of the airway is gradually performed to fully lock the rib graft into the cricoid cartilage split. The balloon size is calculated by adding 3 mm to the outer diameter of the age-appropriate endotracheal tube. Correct graft position and alignment with the laryngeal lumen are then confirmed with a right-angle probe prior to the removal of the safety suture.
Table 1: Preoperative Patient Data.
| Code | Age (Yr) | Gender | Diagnosis | Previous Surgical Interventions |
|---|---|---|---|---|
| 1 | 19 | Male | PGS | • Arytenoidectomy • PGS slicing and balloon dilation • Tracheostomy decannulation |
| 2 | 12 | Male | PGS | • PGS slicing and balloon dilation |
| 3 | 17 | Female | SGS (grade 2) | • SGS slicing and balloon dilation • SGS Bugbee cauterization |
| 4 | 12 | Male | SGS (grade 2) + PGS | • SGS slicing and balloon dilation • PGS slicing and balloon dilation • Tracheostomy decannulation |
| 5 | 11 | Male | PGS | None |
PGS = posterior glottic stenosis; SGS = subglottic stenosis.
Nasotracheal intubation is performed under endoscopic guidance, and the patient is transferred to the intensive care unit (ICU). One week later, the patient undergoes a second-look procedure with dexamethasone administration over 48 hours prior to the planned extubation day. First, the presence of an air leak around the endotracheal tube is confirmed. Then, the patient is extubated, and the graft position and mucosal healing are evaluated. The patient is then temporarily re-intubated with a smaller-sized endotracheal tube to be extubated in the ICU.
Results
Five patients underwent EPCS/RG with a balloon-assisted rib graft placement in our tertiary referral center. Their ages ranged from 11 to 19 years old. Two patients were diagnosed with comorbidities. One patient had a seizure disorder, and another patient had inflammatory bowel disease with chronic anemia. Four of the five patients were male. The patients’ demographics, diagnoses, and previous surgical histories are shown in Table I. None of the patients had a pre-existing tracheostomy, and the insufflation technique was applied to administer intraoperative ventilation in all patients. One patient developed sedation withdrawal syndrome, which was conservatively managed by gradual reduction of the sedation dosage. No postoperative complications were observed in the remaining patients. The length of hospital stay ranged from 12 to 17 days (mean = 14.60, standard deviation [SD] = 1.82).
View the video of the technique described here.