Introduction
Pediatric endoscopic sinus and skull base surgery is challenging due to narrow anatomical confines, variable pneumatization of the paranasal sinuses, inter-carotid distance, and limited instrumentation. With the refinement of endoscopic surgical techniques and the development of new instruments in otolaryngology, however, the specific challenges of pediatric skull base surgery may be overcome with the adaptation of these techniques and the adoption of new instruments (Int Forum Allergy Rhinol. 2018;8:955–958; Laryngoscope. 2012;122:1661–1669). The objective of this article is to present a novel technique using endoscopic ear instrumentation and a modified Draf III approach for the resection of a nasal dermoid cyst with an intracranial component that is applicable to the pediatric patient without frontal sinus pneumatization and with narrow nasal cavities.
Explore This Issue
July 2022Method
A case of the pediatric nasal dermoid cyst was identified, informed consent was obtained, and exemption from the institution review board was given. The patient presented at age 18 months with a nasal dorsum lesion with protruding hair. Computed tomography (CT) and magnetic resonance imaging (MRI) demonstrated a nasal dorsum dermoid cyst, a defect in the foramen cecum, and an intracranial dermoid cyst within a bifid crista galli. The intracranial lesion measured 5 to 6 mm and appeared extradural; however, the nasal and frontal bones were fused, and therefore no tract could be identified and followed from the nasal dorsum lesion to the intracranial lesion. To avoid nasal bone osteotomies, the nasal dorsal lesion was excised through a direct approach, and resection of the intracranial lesion was planned for a later date. Following removal of the lesion on the nasal dorsum, subsequent MRI imaging revealed rapid progression of the intracranial lesion to a size of 10 mm. Therefore, the patient’s family and the surgical teams agreed to proceed with the endoscopic removal of the patient’s intracranial dermoid cyst at the age of 24 months.
Surgical Technique
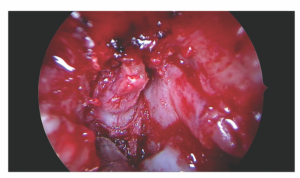
The procedure began with standard bilateral maxillary antrostomies and spheno-ethmoidectomies. To adapt for the narrow nasal cavities, 2.7 mm pediatric 0° and 30° endoscopes were used, while keeping a standard 4-mm blade for the microdebrider. The House stapes curette was used to facilitate dissection in the sinuses. After skeletonizing the skull base and orbit, bilateral superior and lateral anteriorly-pedicled mucosal flaps were elevated from the frontal process of the maxilla using a Beaver blade and Rosen round knife with integrated suction (Int Forum Allergy Rhinol. 2018;8:955–958). The bone over the lacrimal sac was then resected with a 2-mm otologic drill and 1-mm Kerrison rongeur until the lacrimal sac was exposed to maximize the working corridor laterally. The initial steps of an outside-in endoscopic modified Lothrop procedure were then initiated to expose the dermoid cyst (Laryngoscope. 2012;122:1661–1669). Using the suction round knife, a continuous incision was made from the lateral nasal wall to the septum in a coronal plane at the level of the most anterior portion of the frontal beak. This allowed identification of the first olfactory fascicle bilaterally by reflecting the mucosal flaps posteriorly. The superior septectomy was completed, and the frontal bone just anterior to the cribriform plate was removed using the drill. After thinning out the non-pneumatized frontal bone, the capsule of the dermoid cyst was identified. A Beaver blade was used to longitudinally divide the perpendicular plate of the ethmoid, which had not yet ossified, exposing the cyst within the bifid crista galli (Figure 1). The cyst was dissected circumferentially using the stapes curette and suction round knife, followed superiorly to the dura as it split the crista galli. This allowed for complete macroscopic removal of the dermoid cyst as it was detached from the dura of the frontal lobes and the ventral inter-hemispheric fissure. The remaining adherent capsule of the lesion was cauterized with bipolar cautery. A very faint cerebrospinal fluid leak was repaired with an underlay and overlay of synthetic dural matrix, followed by dural sealant. Septal cartilage was replaced, and the previously elevated mucosal flaps were then repositioned in their anatomic location to reconstruct the septum and cover exposed bone.
Results
The patient was admitted to the inpatient unit for monitoring of vital signs, neurological signs, and clinical evolution. He was put on a 10-day course of oral Augmentin and discharged on the second postoperative day. Given his young age, the patient was brought back to the operating room two weeks later for debridement of the nasal cavities. No evidence of cerebrospinal fluid leak was identified. At his two-month postoperative visit, the patient continued to do well, and there was no evidence of edema, crusting, or purulence on nasal endoscopy.