INTRODUCTION
The parapharyngeal space is an inverted, cone-shaped potential space extending from the skull base to the greater cornu of the hyoid. Early and small abscesses may resolve with antibiotic treatment; however, surgical drainage of the abscess is often necessary for definitive treatment and to obtain tissue for microbiological and histological testing. Parapharyngeal abscesses are usually drained using an external transcervical approach or an intra-oral approach. For abscesses that are centered around the skull base and superior to the level of the soft palate, a transnasal endoscopic route is a feasible approach (Eur Arch Otorhinolaryngol. 2005;262:722-730). Caution needs to be taken to avoid critical structures such as the Eustachian tube and carotid arteries, however. We demonstrate here a safe technique for transnasal endoscopic drainage of parapharyngeal abscesses.
Explore This Issue
July 2024METHODS
Informed consent was obtained from the patient. Videos and images were de-identified. Institutional review board review was not required based on institutional policy.
A 41-year-old Indian male with poorly controlled diabetes mellitus presented to our hospital with severe right-sided headaches. He had no subjective ear complaints. Examination showed fullness in the right fossa of Rosenmüller, right vocal fold palsy, and right tympanic membrane perforation with granulation tissue and otorrhea. Magnetic resonance imaging (MRI) of the neck and skull base confirmed the diagnosis of right malignant otitis externa with right-sided central skull base osteomyelitis. Mucosal biopsies from the right fossa of Rosenmüller revealed benign histology and tissue culture that grew Staphylococcus aureus. Swab cultures from the right ear grew Candida orthopsilosis and parapsilosis. The patient was treated with a one-week course of intravenous ceftazidime, followed by a five-week course of oral moxifloxacin, and six weeks of oral fluconazole concurrently based on infectious disease specialist recommendations. His headache resolved with treatment, and repeat otoscopy showed resolution of the otorrhea and spontaneous closure of the tympanic membrane perforation. His diabetes was controlled medically, with the improvement of his glycosylated hemoglobin from 11.2% to 7.5% six months later.
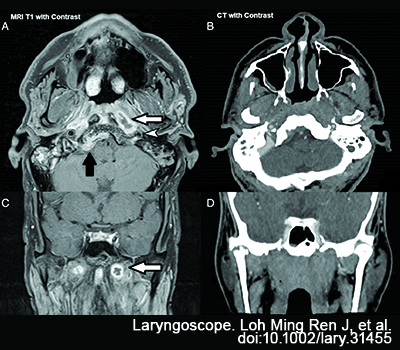
Figure 1. (A) T1-weighted MRI with contrast showing the left upper parapharyngeal abscess (white arrow), the relationship to the left internal carotid artery (white arrowhead), and the right cerebellomedullary abscess (black arrow). (B) CT with contrast, which shows nasopharyngeal asymmetrical prominence but no hypodense collection or rim enhancement. (C) T1-weighted MRI in coronal view, showing the left upper parapharyngeal abscess (white arrow). (D) CT with contrast coronal view.
An interval MRI scan done six months later showed radiological progression of his skull base osteomyelitis to the left, with a new 2.1 × 1.2-cm rim-enhancing abscess in the left nasopharynx and intracranial spread from the clivus to the cerebellomedullary cistern on the right. Computed tomography (CT) scans of the posterior nasal space, with IV contrast, were obtained for surgical planning and image guidance. Unlike the MRI images, the abscess cavity was not well defined on CT and did not have the typical hypodense, rim-enhancing appearance expected of an abscess (Fig. 1). The patient had no symptoms and no rise in inflammatory markers despite radiological progression. Nasoendoscopy was unremarkable, with no visible nasopharyngeal bulge or purulence. Otoscopy was normal on the left but showed a clear effusion on the right. Infectious disease physicians and neurosurgeons were consulted, and an urgent, culture-directed antimicrobial treatment was advised, to arrest the intracranial spread. The patient underwent transnasal endoscopic drainage of the left nasopharyngeal abscess and right tympanocentesis.
TECHNIQUE
Radiographic measurements from the axial cuts were taken between the depth from the mucosal surface to the anterior abscess cavity wall (9 mm), the posterior-lateral wall (31 mm), and the internal carotid artery (33 mm). On coronal sections, the relationship between the abscess cavity and the sphenoid sinus floor and medial pterygoid plates was noted.
The surgery was conducted under general anesthesia. The StealthStation S7 (Medtronic, Minneapolis, Minn., USA) system was used for image guidance. The postnasal space was washed with half-strength iodine followed by normal saline to minimize contamination with commensal flora. Septoplasty, posterior septectomy, or inferior turbinectomy can be considered to improve endoscopic and instrument access but was not necessary in this case.