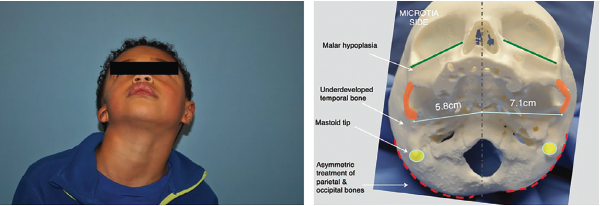
Figure 1. Left: preoperative image demonstrating degree of hemifacial microsomia highlighted by deficient mastoid and asymmetric midface and mandible. Right: 3D-printed skull highlighting these changes at the bony level.
Explore This Issue
March 2022© Laryngoscope. Kimura, et al.doi:10.1002/lary.29823
Using the 3D-printed model, a standard PPE implant was placed while visualizing the contralateral ear at different angles. Ideal positioning was based on a location that achieved the greatest amount of symmetry to the contralateral ear in three dimensions, including both the height of the upper third of the ear (on profile and frontal views), anterior/posterior positioning (profile), and projection of the lower third of the ear (frontal).
Once ideal positioning was determined, a silicone putty mixture was placed onto the model and manipulated by adding or removing material to support the position of the PPE implant at the ideal AOP. At that point, the silicone was allowed to harden. Next a 3-mm punch biopsy tool was used to take measurements at three separate places on the mold (helical root, common crus, and the base of the conchal bowl). This process was repeated an additional two times to ensure consistent measurements.
Once ideal position and augmentation of the ear were determined, facial landmarks were sketched onto clear plastic as a template for intraoperative positioning. Landmarks included the microtic ear, lateral canthus, lateral nasal sidewall, alar crease, and oral commissure. This process effectively created a template mask to help replicate placement (in two dimensions) on the day of surgery, while the depth of the silicone putty mold measurements determined projection in 3D of the lower third of the ear.
Intraoperative Application: On the day of surgery, the template mask previously created during preoperative planning was used to mark the ideal placement of the ear. This was performed prior to sterilization and draping of the patient. Next, the template was placed between two sterile transparent dressings, which allowed for frequent verification of positioning once a sterile field was created. The measurements taken from the silicone wedge during the preoperative planning session were used to augment the PPE auricular framework (by adding from a separate PPE block) and appropriately project the lower third of the ear.
Patients were routinely seen in follow-up three to five days postoperatively for removal of a protective head dressing, and again one week later for removal of silicone casting material secured over the neo-auricle. Intralesional corticosteroid was injected as needed at the surgeon’s discretion around three to four weeks later to areas that appeared to demonstrate excessive edema. Patients were instructed to protect the ear at night with the use of a removable silicone cast for several weeks.
Results
Hemifacial microsomia presents a unique challenge in microtia repair due to the particular anatomic abnormalities that result from a deficient mastoid and asymmetric midface. This study aims to introduce a new concept, the AOP, which should be identified in all patients with hemifacial microsomia undergoing microtia repair. Matching the AOP when reconstructing the microtic ear allows for the optimization of aesthetic outcomes, in particular along the frontal view. We describe a 3D imaging protocol that can be useful in predicting the degree of mastoid deficiency present, and can help augment the lower third of the neo-auricle to accommodate this deficiency. As technology continues to improve, it is important for the field of facial plastics and reconstructive surgery to rely more on quantitative data and calculable measurements in order to achieve optimal outcomes more consistently.