A bright red patch on the face of an infant might be a hemangioma, but what kind? A panel tackled the topic here on Jan. 26 at the Triological Society Combined Sections Meeting.
Stephen Conley, MD, a pediatric otolaryngologist at Children’s Hospital of Wisconsin, said hemangiomas in pediatric patients pose a special challenge because the proper way to proceed might not be clear immediately. “Their behavior has made it difficult to predict the need for treatment,” he said.
Carol MacArthur, MD, associate professor of otolaryngology-head and neck Surgery at the Oregon Health & Science University, urged biopsies when doctors aren’t sure about the type of a hemangioma. Congenital hemangiomas and other types may bear similarities to the less serious infantile hemangiomas, but there are key differences.
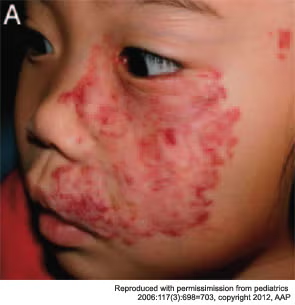
Maxillary segmental hemangiomas.

“They often initially look like an infantile hemangioma,” Dr. MacArthur said, “but on closer inspection have some differences and often act very differently. One of the main take-home messages I would like to convey is when things aren’t going in a typical fashion, think about doing a biopsy.” That will help differentiate infantile hemangioma, which are GLUT 1-positive, from the others, which are all GLUT 1-negative.
Rapidly involuting congenital gemangiomas (RICH) are fully formed at birth and rapidly collapse and fade within six to 12 months after birth, likely not needing medical therapy. But ulceration during involution might call for excising them earlier, Dr. MacArthur said.
Non-involuting congenital hemangiomas (NICH) are more rare, have a raised surface, and don’t respond to medical therapy. They might need to be excised, with embolization prior to the operation.
Kaposiform hemangioendothelioma (KHE) is a more aggressive, infiltrating vascular mass and can lead to Kasabach-Merritt Syndrome, which involves thrombocytopenia and microangiopathic hemolytic anemia and can have a mortality rate of up to 30 percent. Vincristine is most commonly used to treat these.
Tufted angioma can also lead to K-M Syndrome and treatment can include propranolol, although often at high doses, as well as vincristine and steroids.
Robert Yellon, MD, co-director of pediatric otolaryngology at the Children’s Hospital of Pittsburgh, said PHACES Syndrome, a neurocutaneous syndrome, is “underappreciated and underdiagnosed.” “When these occur, they’re important because the kids can be very sick because of cardiac and intracranial and vascular anomalies,” Dr. Yellon said.
The syndrome name is an acronym that captures its many facets: posterior fossa brain malformation, hemangiomas, arterial cerebrovascular anomalies, cardiovascular anomalies, eye anomalies, and sternum-ventral development defects.
Diagnosis can be confirmed by a segmental infantile facial hemangioma on the face or scalp longer than 5 cm, a segmental hemangioma with no precise distribution across the anatomy, and at least one related feature beyond the skin such as structural brain and cerebral vascular anomalies.
In a 2006 study of 1,096 hemangiomas (J Med Genetics. 140:975-986), 25 cases, or 2 percent, were found to be PHACES. Of the segmental facial hemangiomas, 20 percent were PHACES cases. Ninety percent of the PHACES cases occurred in females.
Because of the complex nature of the syndrome, Dr. Yellon recommended a multidisciplinary approach to treatment, with input from dermatology, cardiology, cardiothoracic surgery, endocrinology and other departments.
A Promising Treatment
Anna Messner, MD, professor and chair of otolaryngology-head and neck surgery and pediatrics at Stanford University, sang the praises of propranolol, a non-selective Beta adrenergic antagonist that has proven to be effective in hemangioma treatment, with the first effects visible in just a day or two.
The use of propranolol began with two children being treated with the therapy for obstructive hypertrophic cardiomyopathy, when the effects on their hemangiomas was noticed. After the same thing was seen in nine more children, the observations were related in a June 2008 letter to the editor in the New England Journal of Medicine, Dr. Messner said.
Dr. Messner said it’s unclear how it works, but it’s suspected that vasoconstriction, bringing about decreased blood flow to the hemangiomas, might be partially the cause. The major effect might be the inhibition of catecholamine’s stimulation of vascular endothelial growth factor. Also involved might be the down-regulation of other cytokines that promote formation of new blood vessels and the prevention of hemangioma stem cell differentiation into endothelial cells or pericytes.
She said that possible side effects include bradycardia, hypotension, bronchospasms and hypoglycemia, among others. There have been no documented cases of serious side effects but because of the hypoglycemia risk, propranolol should be given with food.
In a randomized, placebo-controlled trial of 40 children aged nine weeks to five years, propranolol brought about a 60 percent reduction in the volume of hemangiomas after 24 weeks, while there was less than a 20 percent reduction in the placebo group (Pediatrics. 2011;128:e259-e266).
The case that propranolol is effective has been essentially settled, she said. “My opinion is at this point doing more random controlled trials on propranolol versus steroid is the equivalent of doing a trial to see whether a parachute will help someone jumping out of a plane,” Dr. Messner said. “It really doesn’t make much sense.”
Leave a Reply