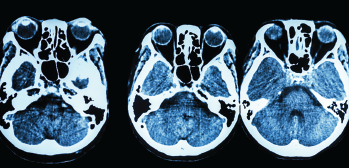
How valid is the 5-factor modified frailty index (mF1-5) as a predictor of perioperative morbidity and mortality in patients undergoing skull base surgery?
BOTTOM LINE
Frailty as measured by the 5-factor mF1-5 is shown to be significantly associated with life-threatening postoperative morbidity, mortality, and length of stay following skull base surgeries.
BACKGROUND: Frailty is a state of diminished physiological reserve that has been associated with increased risk of postoperative morbidity and mortality. Given the current global demographic transition toward older age, an effective preoperative risk stratification tool assessing frailty of patients undergoing skull base surgery could help predict postoperative complications.
STUDY DESIGN: Cross-sectional study.
SETTING: Department of Otolaryngology–Head and Neck Surgery, Rutgers Robert Wood Johnson Medical School, New Brunswick, N.J.
© Puwadol Jaturawutthichain / shutterstock.com
SYNOPSIS: Researchers accessed the National Surgical Quality Improvement Program database and identified 17,912 patients (44.9% male, mean age 52.0 years) undergoing skull base surgeries between 2005 and 2018. Patients’ frailty scores were calculated using the mF1-5, with variables including non-independent functional status (requiring assistance for daily activities), diabetes mellitus, chronic obstructive pulmonary disease or pneumonia, congestive heart failure, and hypertension requiring medication. Approximately 45.6% of patients had at least one frailty-qualifying factor, and the overall complication rate for the cohort was 11.4%. Results showed that as mF1-5 scores increased, overall complication rates rose in a stepwise manner (8.7% to 30.2%); the odds of life-threatening systemic complications increased approximately 42.8% for each unit rise in the score. Frailty was not predictive of complications in the anterior fossa cohort, suggesting that surgical advancement here may have tempered operative risk for these patients. Authors conclude that frailty as defined by the mF1-5 may have a potential use in identifying high-risk candidates, facilitating perioperative planning, and optimizing outcomes. Study limitations included its retrospective design and potential selection bias of the database.
CITATION: Henry RK, Reeves RA, Wackym PA, et al. Frailty as a predictor of postoperative complications following skull base surgery. Laryngoscope. 2021;131:1977-1984