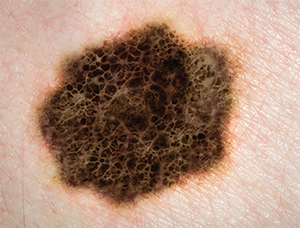
Melanoma.
© AUSTRALIS PHOTOGRAPHY; SHERRY YATES YOUNG/SHUTTERSTOCK
The rate of skin cancer occurrence in the United States is “climbing at epidemic proportions,” said Cecelia Schmalbach, MD, MSc, professor and vice chair of otolaryngology-head and neck surgery at Indiana University School of Medicine in Indianapolis. In 1960, the incidence of melanoma was one in 600 in the United States; in 2012, it was one in 36. The disease is more common in men; after age 40, it’s twice as common in men than in women. But, in one of four new cases, the patient is younger than 40. Melanoma is also the most common cancer in women aged 25 to 29 and the second-most common in women aged 30 to 34.
Explore This Issue
November 2016Mortality from melanoma has increased by approximately 3% since 2004, and more than 10,000 people will die from the disease in 2016. According to the National Cancer Institute, 40% to 50% of Americans will have at least one basal cell or squamous cell cutaneous carcinoma by age 65.
A surgeon’s or center’s experience, as well as a quickly changing evidence base, can influence decisions made in the treatment of skin cancers. Panelists at the American Academy of Otolaryngology-Head and Neck Surgery Foundation Annual Meeting discussed how they and their tumor boards would handle a variety of cases.
Case 1: Melanoma on the Scalp
A 55-year-old man presented with a newly diagnosed desmoplastic melanoma on his scalp; he had undergone a punch biopsy by a dermatologist. The lesion was thought to be a T2N0M0 desmoplastic melanoma.
Carol Bradford, MD, professor of otolaryngology and executive vice dean of academic affairs at the University of Michigan Medical School in Ann Arbor, said that a history and physical would be acceptable for work-up, but noted that a wide local excision and a sentinel node biopsy would be the best staging study.
For Stage 1 and 2 melanomas, the National Comprehensive Cancer Network (NCCN) guidelines suggest just a history and physical, with imaging performed only for specific symptoms. In this case, even though desmoplastic tumors have a lower rate of positive nodes, Dr. Bradford advised considering a sentinel node biopsy. “You’re not really biopsying the whole thing and there are very few true, pure desmoplastic melanomas, so this patient would still be eligible for sentinel lymph node biopsy,” she added. She said that the surgeon should have a conversation with the patient to make it clear that while the biopsy is recommended, the patient is not certain to benefit from it.
Jeffrey Liu, MD, associate professor of otolaryngology-head and neck surgery and director of the division of head and neck oncologic surgery at the Lewis Katz School of Medicine at Temple University and Fox Chase Cancer Center in Philadelphia, said he would recommend a 2-cm margin on this tumor, rather than a smaller margin, due to the biology of the disease. It has a high local recurrence rate and can actually be much more difficult to control than traditional melanomas, he said, adding that he would perform mapping biopsies in the office.
Steven J. Wang, MD, interim director of otolaryngology-head and neck surgery at the University of Arizona in Tucson, agreed with the larger, 2-cm margin for this case. “The key thing here is, on the scalp, I see no downside to favoring a larger margin,” he added.
Following surgery, the dermatopathologist’s report showed deep invasion—7 mm down to Clark’s level 5. While the surgery had achieved negative margins, Dr. Liu said that he would still recommend adjuvant radiation therapy to maximize the chance for locoregional control. “By every measurement, this is a high-risk cancer patient,” he added.
Dr. Bradford didn’t agree that this was a clear-cut case for adjuvant therapy. There’s no prospective data that adjuvant radiation therapy will offer a patient improved overall survival. “However, this is a worrisome lesion,” she added. “I think adjuvant radiation merits a discussion in multidisciplinary, tumor-board fashion. But you have attained clear margins, fairly significantly clear margins, so I personally am a little bit on the fence about radiation in this circumstance.”
Case 2: Third Diagnosis of Melanoma
A 65-year-old English professor with a history of a T2M0M0 right post-auricular melanoma had been treated in 2008 with wide local excision and sentinel node biopsy, which was negative. Two years later, he presented with melanoma in situ; again, it was resected with negative margins. In 2016, he presented with a melanomic lesion biopsied at an outside center and had a melanoma diagnosis for the third time. A repeat punch biopsy confirmed the lesion as melanoma in situ. The patient experienced no symptoms at all.
He was scheduled for a wide local excision, but on preoperative X-ray, a mass was found in his chest and found to be metastatic melanoma to the right lung. The panelists agreed that realistic options at this point included ipilimumab, PD-1 blockers, and combination therapy.
With this patient, Dr. Wang said he would lean a lot on his medical oncologist.
“This is a field that has changed dramatically in the last few years, and it’s hard to keep up with everything that’s going on,” he said, adding that he would discuss clinical trials as well as standard therapy with this patient.
Dr. Liu agreed, saying, “These are the exact kind of patients [in whom] we know prognosis is poor, but we may address that prognosis tremendously with a new agent.”
The NCCN guidelines recommend offering clinical trials for treating unresectable metastatic melanoma. “The take-home message I want you to remember,” Dr. Schmalbach said, “is that we have a lot of options with respect to metastatic melanoma, but there is never going to be one single magic bullet. That’s because there are multiple different genetic mutations that are associated with melanoma, as well as 30% of patients who don’t have a detectable mutation.”
Case 3: Merkel Cell Carcinoma on the Head
A 67-year-old male presented with a rapidly growing 3-cm, biopsy-proven Merkel cell carcinoma (MCC), staged as T2N0M0, on the top of the head.
Dr. Liu, who oversaw the case, said one of three sentinel lymph nodes was positive, so the patient was upstaged to a T2N1 cancer. He pointed out the deeper understanding of MCC that’s evolved over the years: It’s now known that the disease is “exquisitely radiosensitive and quite treatable with radiation. The question is how much surgery should we give in addition to the radiation for treatment.”
The NCCN guidelines offer up multiple options for how to approach these patients and, in this case, the panel was split on whether to perform a completion lymphadanectomy.
We have a lot of options with respect to metastatic melanoma, but there is never going to be one single magic bullet … because there are multiple different genetic mutations that are associated with melanoma. —Cecelia Schmalbach, MD, MSc
An audience member asked why a sentinel node biopsy is necessary if radiation would be performed anyway. “The reason for the sentinel node biopsy is that it focuses the field of radiation into where it’s positive,” Dr. Wang said. This study is helpful for midline lesions, which could drain to either side. Determining laterality can spare unnecessary radiation toxicity. “That would be my argument as to why sentinel node biopsy still has a role,” he added.
Dr. Bradford said that, at the University of Michigan, the recommendation would be to perform a parotid and neck dissection and then radiate according to the risk tumor burden and the number of positive nodes. But, she said, there is no hard data to go on, largely because Merkel cell carcinoma remains a fairly rare and unusual malignancy. She hopes cohort data, at least, becomes available to better guide physicians in how to treat these patients.
She acknowledged that, at this point, “I don’t think [Merkel cell carcinoma] is easy to understand.”
Thomas Collins is a freelance medical writer based in Florida.
Take-Home points
- The incidence of melanoma in the U.S. in 2012 was one in 36 people, a significant increase over the 1960 rate of one in 600.
- Desmoplastic melanomas have a high local aggression rate, so wide margins are often the best option for treatment.
- For patients with unresectable metastatic melanoma, the best therapeutic option might be a clinical trial.
- NCCN guidelines put forth many options for the treatment of Merkel cell carcinoma, but there still is usually a role for sentinel node biopsy and radiation in these cases.
