SAN DIEGO—A panel of experts on facial plastic and reconstructive surgery offered words of wisdom and cautionary tales about treating the aging face in a session at the 2017 Annual Meeting of the Triological Society, held in conjunction with the Combined Otolaryngology Spring Meetings.
The panel touched on the uses of autologous fat grafting, the do’s and don’ts involved in aging face cases, the risks of overzealous and inappropriate filler use, and the challenge in surgery of overcoming a bad result from filler use that has gone awry.
Autologous Fat Transfer

An injection of autologous fat, shown here, can bring many advantages to the aging face.
© Courtesy of Travis Tollefson, MD, MPH
Travis Tollefson, MD, MPH, associate professor and director of facial plastic and reconstructive surgery at the University of California, Davis, said that use of autologous fat transfer is expanding. This approach can be helpful in areas of the aging face that become a bit smaller due to the loss of natural fat.
“Autologous fat grafting … is something that we’ve transferred from the aging face or the cosmetic world into the reconstructive world at a high pace,” he said. “You’ll find a lot of reconstructive cases, as well as aging face cases now, where autologous fat plays a big role in the restoration of volume of soft tissue…. It’s very clear that we can fill in areas and combine autologous fat grafting or fillers with more traditional aging face surgeries.”
Compared with fillers, autologous fat can produce a permanent result. The advantage of synthetic fillers, however, is that they can be injected in the office with little down time after the injection, he added. “The other benefit of the fillers… is that you can place them in the different layers more accurately because they are smooth, and there are different visco-elastic characteristics that allow you to choose the filler that you want to use for the layer.”
Also, in the case of hyaluronic acid, the effects can be reversed if the outcome isn’t acceptable, he said. “With fat transfer, we don’t have a reversible technique, so if you have excess fat in an area,” surgery is required to fix it, he said.
While the risks associated with the use of fillers are low, they can involve a risk of blindness when used around the eye, as well as skin necrosis from vascular infarcts in certain situations, said Dr. Tollefson. “These are too high-risk for me to use in most danger areas, so I do choose autologous fat in most of those cases,” he added.
Embracing an Otolaryngology Foundation
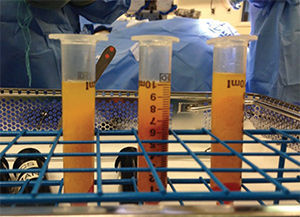
Autologous fat, shown as centrifuged fat.
© Courtesy of Travis Tollefson, MD, MPH
J. Madison Clark, MD, associate professor of facial plastic and reconstructive surgery in the department of otolaryngology at the University of North Carolina in Chapel Hill, outlined five points to his approach to the aging face. “My number one goal is to be safe,” he said. He also strives for a natural result; to address facial movement, which he called the “fourth dimension”; to manage expectations properly; and to handle each case ethically.
“‘Cash,’ to me, is the most dangerous four-letter word,” he said. It can often be the primary driver in decision-making for a facial plastic surgeon or otolaryngologist, and he called it “a very dangerous slope to go down.” He said that his philosophy involves marketing that relies almost exclusively on word of mouth rather than advertising. He drew a distinction between education and selling: “We are selling what we do [not only] by producing good results, but also by educating the patient,” he added.
He encouraged the audience to “embrace your ENT foundation.” He said that some facial plastic surgeons attempt to distance themselves from this foundation. “I embrace my ENT training with pride with my patients, and feel strongly that this dual board certification is precisely what sets us apart from the other specialties that perform plastic surgery on the face,” he said.
He added that his more well-informed patients tell him that his combination of otolaryngology and facial plastic and reconstructive surgery training is why they sought him out for cosmetic surgery.
Filler Misuse
Stephen Park, MD, vice chair of otolaryngology-head and neck surgery in the facial plastic and reconstructive surgery division at the University of Virginia in Charlottesville, said that the temptations are great for some in the field to misuse fillers. The lures of cash “are real,” he said. “If you have some Restylane or other filler, it is just tempting and almost seductive to fix small depressions with a little injection in the office,” he said.

These images show a case handled by Stephen Park, MD, that involved a filler injection gone awry and his surgery to correct nose-tip irregularities.
© Courtesy of Stephen Park, MD
Most of the time, fillers work well and things go smoothly. But when things go wrong, they can have devastating consequences, he said. One patient, a 30-year-old woman, came to him after she underwent an injection procedure with another physician that would, she had hoped, give her a stronger profile. The first injection went poorly, leaving irregularities on the tip of her nose. Then, Dr. Park said, someone tried to fix this with yet another injection. The result was loss of skin, scarring, and further distortion. This deformity was then permanent—and emotionally devastating for the patient. That’s when she went to see Dr. Park. This kind of situation puts the patient and the surgeon in a difficult position, he said. The decision, he said, is sometimes to “go big or go home.”
“I don’t think you can do something endonasally or something simple in the office to fix it,” he said. The patient opted for a forehead flap procedure, and Dr. Park ended up achieving a satisfactory result.
Fillers are often a terrific solution to small contour problems, he said. “The reality is that, occasionally, it can lead to terrible complications that are life changing.”
Thomas R. Collins is a freelance medical writer based in Florida.
Take-Home Points
- Autologous fat injection now plays a prominent role in the restoration of soft tissue volume.
- Autologous fat can produce permanent results but is not reversible short of surgery, while hyaluronic acid can be reversed without surgery if the effects are not desirable.
- Cash as the primary driver in decision-making for facial plastic surgeons can be a “slippery slope.”
- The best kind of marketing may be to produce good results and to educate patients.
- Fillers used overzealously or inappropriately can put surgeons in a difficult “go big or go home” scenario.